Reprod Biol Endocrinol:拮抗剂周期的黄体期添加三妥瑞林可优化ART的结局
2020-07-24 MedSci原创 MedSci原创
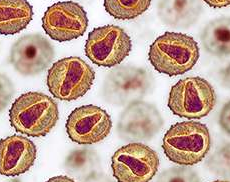
由于子宫内膜中存在GnRH受体,在体外受精方案中黄体期添加GnRH类似物很少被提出。本研究旨在评价在短效拮抗剂周期中添加三羟色胺的效果,与仅补充孕酮的周期相比。
由于子宫内膜中存在GnRH受体,在体外受精方案中黄体期添加GnRH类似物很少被提出。本研究旨在评价在短效拮抗剂周期中添加三羟色胺的效果,与仅补充孕酮的周期相比。
疗效的次要目标是妊娠率和植入率,以及OHSS风险的安全性。该研究是一项前瞻性、随机性、开放性研究,于2013年7月至2015年10月在两个独立的中心进行。将患者分为三组:a)常规拮抗剂方案,仅使用黄体酮;b)拮抗剂方案,黄体三联为多次注射,c)拮抗剂方案,黄体三联为单栓。
结果,共有1344名患者完成研究,786名35岁以下,558名35岁以上。当黄体期加入三甲双胍时,无论是否作为单栓或五次注射,阳性HCG结果、临床妊娠率和分娩率都增加。这种增加对妊娠率和分娩率均有统计学意义。妊娠和分娩之间的统计学差异在有无黄体三联素时达到p<0,01。没有观察到OHSS风险的增加。
总之,从这项大型研究来看,黄体期补充的概念应该被重新审视。从我们的研究看来,在拮抗剂周期的黄体期添加三妥瑞林,无论是作为单次栓剂还是使用多次注射,都是优化ART结果的好方法。
原始出处:
Francesco M Fusi, Claudio M Brigante, et al., GnRH agonists to sustain the luteal phase in antagonist IVF cycles: a randomized prospective trial. Reprod Biol Endocrinol. 2019 Nov 29;17(1):103. doi: 10.1186/s12958-019-0543-2.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Bio#
31
#ART#
26
#拮抗剂#
39
#PRO#
36
#Biol#
31