CGH: 频繁的排便会增加憩室炎风险
2022-01-26 MedSci原创 MedSci原创
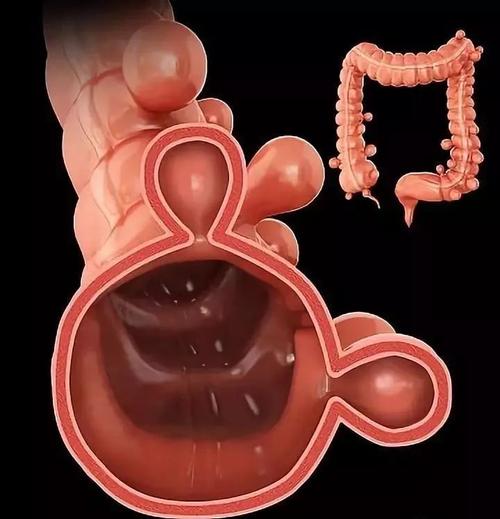
结肠憩室可分为先天性和后天性两种,以后天性为多。憩室的形成,尤其是在左结肠,几乎皆为老化现象,年纪越大,越容易发生。憩室本身并不会造成任何问题,但若其开口被阻塞时,则形成憩室炎。
憩室炎是患者需要入院治疗的最常见的胃肠道疾病之一,也是门诊的主要诊断之一。危险因素包括吸烟、运动不足、肥胖、使用绝经期激素和用非甾体抗炎药(NSAID)等。但是排便习惯对憩室病和憩室炎的影响尚不清楚。长期以来,人们一直认为频繁的排便与无症状的憩室病风险较低有关。但最近的横断面研究发现更频繁的排便与更高的症状性或无症状憩室炎的发病有正相关关系。因此,本项研究试图在美国的两个大型前瞻性队列中评估肠道运动频率和发生憩室炎的风险之间的关系。
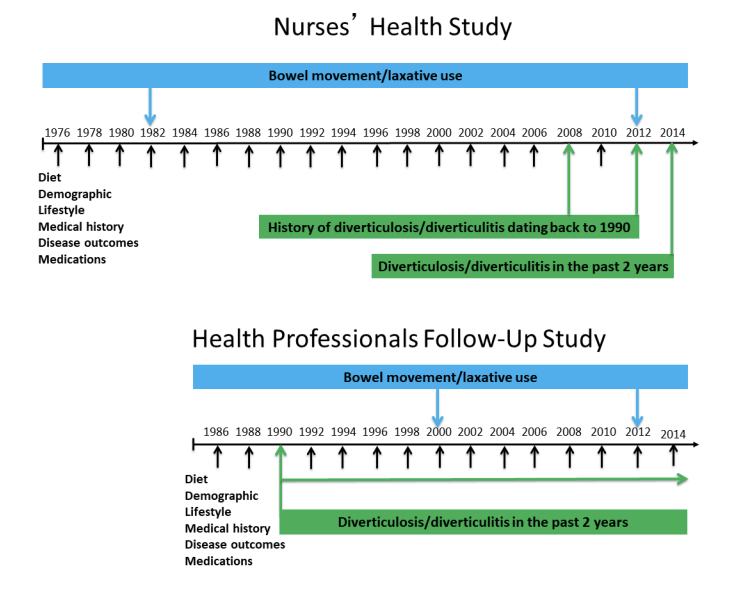
为此,研究人员收集了美国护士健康研究 (NHS) 和健康专业随访研究 (HPFS) 中的参与者的数据资料。在 Cox 比例风险回归模型中使用参与者的病史、生活方式因素和饮食来估计多变量调整后的风险比 (HRs) 和 95% 置信区间 (CI)。最后进行了统计学学上的差异比较。

在 NHS队列超过 24 年的随访时间中,总共包含了1299922人年,共记录了 5214 例憩室炎事件的发生,在 HPFS队列超过14年的随访时间中,总共包括368,661 人年,共记录了390例憩室炎事件的发生。研究结果发现排便频率与憩室炎风险之间存在负相关。在 NHS队列中,与每天排便的女性相比,每天排便超过一次的女性发生憩室炎的HR 为 1.30(95% CI,1.19,1.42),排便频率较低的女性的憩室炎的HR为 0.89(95% CI, 0.82, 0.95;p< 0.0001)。在 HPFS队列中,相应的 HR 为 1.29 (95% CI, 1.04, 1.59) 和 0.61 (95% CI, 0.36, 1.03;p = 0.003)。
因此,本项研究结果证实更频繁的排便似乎是男性和女性继发憩室炎的危险因素,然而,需要进一步的研究来了解可能构成这种关联的潜在机制究竟是什么。
原始出处:
Manol Jovani. Et al. Frequency of Bowel Movements and Risk of Diverticulitis. Clinical Gastroenterology and Hepatology.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#排便#
46
#CGH#
54
#憩室炎#
49
#憩室#
39
学习了新的知识
0