Sci Signal:揭示巨噬细胞识别感染和组织损伤机制
2016-08-31 佚名 生物谷
在我们的细胞周围的微环境中进行巡逻的任务是由巨噬细胞执行的。巨噬细胞是在体内大多数组织中进行巡逻的“卫士”---时刻准备着吞噬入侵的病原体或破坏和修复受损的组织。 在过去10年里,人们普遍认为巨噬细胞能够检测人组织微环境中发生的变化。它们能够观察到病原体入侵和组织损伤,调节为此作出反应的炎性过程来摧毁微生物入侵者、清除和修复受损的组织。但是细胞世界中的这些卫士如何应对感染和组织损伤呢? 在一项
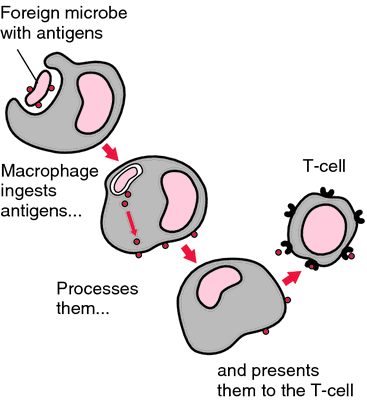
在过去10年里,人们普遍认为巨噬细胞能够检测人组织微环境中发生的变化。它们能够观察到病原体入侵和组织损伤,调节为此作出反应的炎性过程来摧毁微生物入侵者、清除和修复受损的组织。但是细胞世界中的这些卫士如何应对感染和组织损伤呢?
在一项新的研究中,英国诺丁汉大学药学院炎性信号通路专家Anna Piccinini博士和同事们发现巨噬细胞的“摧毁和修复服务”通过部署单个感应器而能够区分这两种截然不同的威胁。因此,它们能够精心安排特异性的免疫反应---当它们遭遇感染时,以炎性分子的形式传递信息;当它们检测到组织损伤时,制造和修饰这种组织中的分子组分。相关研究结果发表在2016年8月30日那期Science Signaling期刊上,论文标题为“Distinct microenvironmental cues stimulate divergent TLR4-mediated signaling pathways in macrophages”。
她的发现可能为未来治疗发生广泛性组织损伤的疾病如关节炎或癌症提供靶标,其中在这些疾病中,炎症发挥着越来越重要的作用。
Piccinini博士说,“尽管我们知道巨噬细胞能够利用单个感应器检测不同的威胁,但是我们从没有真正地理解基于它们遭遇到的威胁类型,它们是否使用相同的或不同的防御策略。有趣的是,我们也正在更好地理解巨噬细胞行为如何影响它们周围的微环境。”
Piccinini博士说,“这项研究为鉴定出这些细胞针对感染和无菌组织遭受的损伤作出的特异性反应时产生的特异性分子事件和在未来可能允许我们发现操纵炎症的特异性靶标铺平道路。”
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#组织损伤#
34
#Sign#
21
#Signal#
25
继续关注
47
很好,不错,以后会多学习
44
#损伤#
28
非常感谢
34
很好,不错,以后会多学习
58
学习了,谢谢了!
42
学习起来
24