JACC:心梗合并房颤老年患者的抗栓治疗,三联还是两联?
2015-10-26 徐媛 MedSci原创
抗血栓治疗急性心肌梗死(MI)和心房颤动(AF)在发病风险更高的老年患者接受冠脉支架置入术(PCI)仍不清楚。本研究评估了适当的抗凝治疗对急性心肌梗死患者房颤与PCI。 研究人员收纳了年龄≥65岁的4959名急性冠脉治疗和介入预后在急性心肌梗死后接受了冠脉支架置入术的网络注册项目患者,且均合并房颤。主要疗效终点为2年时的MACE,包括死亡、心梗或卒中相关的入院。主要安全性终点为2年时因出血再入院
抗血栓治疗急性心肌梗死(MI)和心房颤动(AF)在发病风险更高的接受冠脉支架置入术(PCI)的老年患者中的影响仍不清楚。本研究评估了适当的抗凝治疗对急性心肌梗死患者房颤和PCI的影响。
研究人员收纳了年龄≥65岁的4959名急性心肌梗死和房颤患者,经过急性冠脉治疗和介入术后,进行了网络注册项目。主要疗效终点为2年时的MACE,包括死亡、心梗或卒中相关的入院。主要安全性终点为2年时因出血再入院。根据出院时采用三联或双联治疗进行分层。
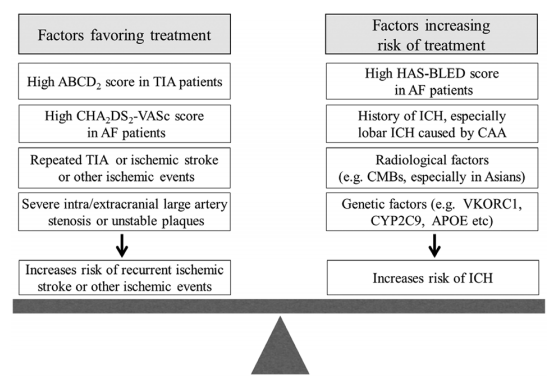
在4959名患者中有27.6%(n = 1,370)出院时接受了三联治疗。与双联(DAPT)相比,三联治疗者MACE发生率相似(调整的HR = 0.99; 95% CI 0.86-1.16);三联治疗者因出血需再入院的发生率升高(调整的HR = 1.61; 95% CI, 1.31-1.97),颅内出血风险升高(调整的HR = 2.04; 95% CI, 1.25-3.34)。全因死亡、心梗再入院和卒中再入院发生率相似。三联治疗组缺血性卒中风险降低,但差异无统计学意义(HR = 0.66; 95% CI, 0.41-1.06)。
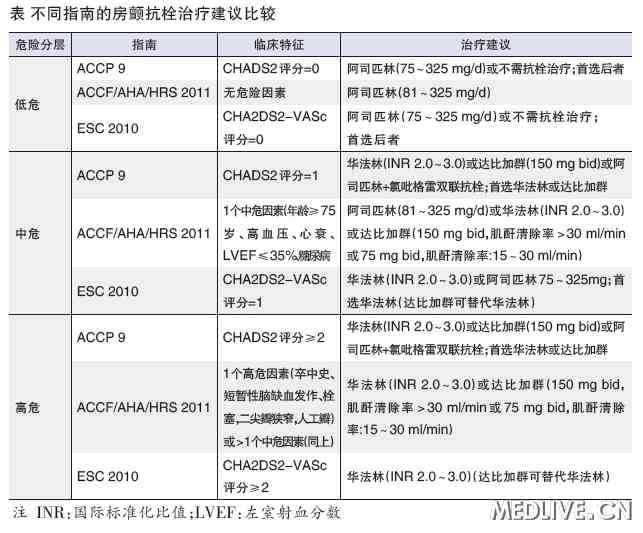
以上研究结果显示:合并房颤的急性心肌梗死患者在PCI治疗出院后三联治疗(阿司匹林+氯吡格雷+华法林)与两联治疗(阿司匹林+氯吡格雷)的2年主要不良心脏事件风险相似,但前者大出血风险更高。
原始出处
Connie N. Hess, MD, MHS.et al.Use and Outcomes of Triple Therapy Among Older Patients With Acute Myocardial Infarction and Atrial Fibrillation.JACC.2015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JACC#
16
#ACC#
28
两联已充分了
46
符合预期
138