Exp Ther Med:眼眶IgG4相关疾病的临床观察
2019-01-31 MedSci MedSci原创
天津市第一中心医院眼科的Wu N等,在Exp Ther Med杂志上发表了一篇研究论文,研究的目的是观察免疫球蛋白G4相关眼眶疾病(IgG4-RODs)的组织病理学变化,总结眼睑IgG4-RODs的临床表现和影像学特征,探讨IgG4-RODs的早期诊断措施。
天津市第一中心医院眼科的Wu N等,在Exp Ther Med杂志上发表了一篇研究论文,研究的目的是观察免疫球蛋白G4相关眼眶疾病(IgG4-RODs)的组织病理学变化,总结眼睑IgG4-RODs的临床表现和影像学特征,探讨IgG4-RODs的早期诊断措施。
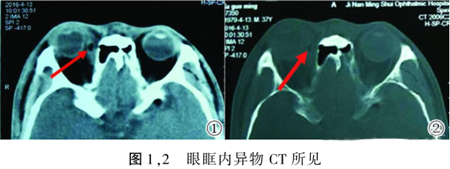
他们在2011年6月至2015年5月期间,招募了天津市第一中心医院眼科的23例非特异性眼眶炎症患者。其中,9名患者血清IgG4的滴度范围为4.58至46.70g / l(参考值,0.03-2.01g / l),平均值为21.93±2.18g / l。值得注意的是,9名IgG4-ROD患者的变化程度不同,但均> 1.35 g / l。同时观察到6例出现眼眶下神经增厚的情况。另外,有3例存在眼外肌增厚症状,1例IgG4-ROD眼眶组织病变的情况是沿下颞隔延伸至左翼腭窝、左骶裂,左上颌窦也受到影响。
该研究表明,下眼眶神经增厚可能是IgG4-ROD的临床特征。因此,作者建议,在临床活检和血清检查的基础上,早期诊断可结合影像学检查、临床表现和实验室检查等,以减少误诊和漏诊。
原文出处:
Wu, N. and F.Y. Sun, Clinical observation of orbital IgG4-related diseases. Exp Ther Med, 2019. 17(1): p. 883-887.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#临床观察#
28
#IgG4#
32
#眼眶#
36
#IgG4相关疾病#
40
#Med#
28
#IgG#
31
好
51
学习了,涨知识了!
55