病例讨论:B超发现肝脏占位一例
2015-12-11 吕鹏 林江 复旦大学附属中山医院放射科
【病史】: 男性,34岁,因外院体检B超发现肝脏占位来我院就诊。患者无腹痛、腹胀、皮肤黄染等不适主诉,体格检查无殊。肿瘤标志物AFP:5.2 ng/ml,CEA:1.02 ng/ml;CA19-9:19.0 U/ml。乙肝两对半 HBsAg(-)HBsAb(+)HBeAg(-)HBeAb(-)HBcAb(+)。 患者入院后行增强CT及MRI检查,图如下:
【病史】:
男性,34岁,因外院体检B超发现肝脏占位来我院就诊。患者无腹痛、腹胀、皮肤黄染等不适主诉,体格检查无殊。肿瘤标志物AFP:5.2 ng/ml,CEA:1.02 ng/ml;CA19-9:19.0 U/ml。乙肝两对半 HBsAg(-)HBsAb(+)HBeAg(-)HBeAb(-)HBcAb(+)。
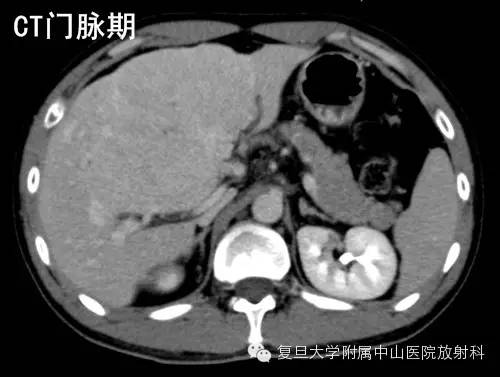
患者入院后行增强CT及MRI检查,图如下:








答案往下
{nextpage}
【CT表现】:
肝脏巨大低密度肿块,增强后动脉期明显强化,门脉期较周围肝实质呈等密度,密度较均匀,动脉期MIP示粗大供血动脉。
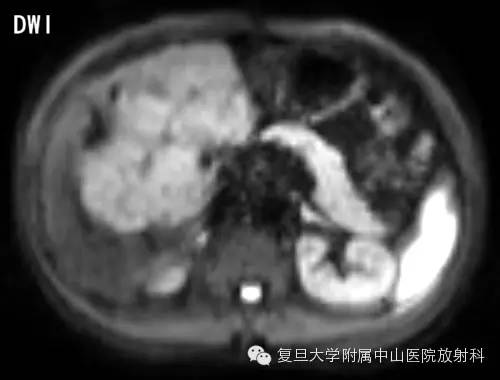
【MR表现】:
T2WI呈稍高信号,T1WI呈稍低信号,DWI呈高信号,病灶中央见疤痕,T1WI及T2WI均为低信号,增强后动脉期病灶明显强化,门脉期及延迟期病灶较周围肝实质呈等至稍高信号,延迟期可见中央瘢痕强化。
【手术所见】:
探查无肝硬化,无腹水,肿瘤位于肝中叶V、IV段,累及部分VIII段,大小约15*12*8cm,界清,无包膜,肝门淋巴结无肿大,门脉主干及左、右分支无癌栓。
【病理】:
巨检:部分肝组织,大小为13.5*13*7cm,切面土黄色,结节状,中央见瘢痕,四周间少许肝组织。
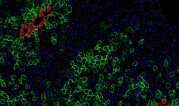
(肝中叶)局灶性结节增生,周围肝G1S0。免疫组化:CK19示胆管增生,CD34血管较丰富,AFP(-), HEPA(++), HBsAg(-),HBcAg(-),HCV(-),HSP70片状(+),GPC3(-),GS地图样(+)。网染(示网状支架存在)。
【讨论】:
肝脏局灶性结节增生(focalnodular hyperplasia,FNH)是一种肝脏的增生/再生病变。FNH由肝细胞、胆管、血管和Kupffer细胞构成,肝细胞的细胞学形态与正常肝组织完全相同。病灶中心常可见纤维瘢痕,向外呈放射状分布,分隔内含有厚壁血管,并将病变分隔为类似于肝硬化的小叶结构。人群中FNH的患病率约为0.9%,并好发于年轻人,男女比例约为1:8。FNH通常是影像学检查偶然发现的。没有症状的FNH通常不需要临床处理,但是对于有症状的患者或者病灶较大时,可以考虑手术切除或化疗栓塞。
典型的FNH在CT平扫时表现为低或等密度,动脉期除了中央瘢痕外病灶表现为均匀明显强化,门脉期及延迟期病灶相对周围肝脏为等密度,中央瘢痕可以呈现部分强化。典型的FNH在MRI的T1WI为等或稍低信号,T2WI为等或稍高信号,中央瘢痕在T2WI为高信号,增强后表现与CT相仿。
FNH的不典型表现如下:
1.没有中央瘢痕,通常见于小于3cm的病变内;中央瘢痕在延迟期为低或等信号,或T2WI为低信号。
2.动脉期强化不明显
3.门脉期或延迟期呈低信号
4.病灶密度不均匀
5.出现假包膜
绝大多数FNH表现典型,易于诊断。极少数FNH会出现上述两条或更多的不典型表现,可能需要与肝细胞肝癌、纤维板层样肝癌、肝细胞腺瘤等病变进行鉴别,此时病灶平扫时的相对等密度/信号及增强后的相对均匀的强化往往是鉴别要点。肝脏的MR特异性造影剂如普美显的应用对FNH的诊断也有一定帮助,由于FNH仍具有正常肝细胞的功能,所以在肝胆特异期表现为等或稍高信号,中央瘢痕表现为低信号。此外,患者AFP水平正常及无慢性肝炎的病史也有助于FNH与肝细胞肝癌鉴别。如果诊断仍然不明确,推荐行病灶穿刺活检。
【参考文献】:
1. Marin D,Brancatelli G, Federle MP et al (2008) Focal nodular hyperplasia: typical andatypical MRI findings with emphasis on the use of contrast media. Clin Radiol63:577-585
2. Asbach P,Klessen C, Koch M, Hamm B, Taupitz M (2007) Magnetic resonance imaging findingsof atypical focal nodular hyperplasia of the liver. Clin Imag 31:244-252
3.Vilgrain V (2006) Focal nodular hyperplasia. Eur J Radiol 58:236-245
4. Hussain SM,Terkivatan T, Zondervan PE et al (2004) Focal Nodular Hyperplasia: Findings atState-of-the-Art MR Imaging, US, CT, and Pathologic Analysis1. Radiographics24:3-17
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#病例讨论#
34
赞一个
132
好学习讲得很好
123
前段时间也收到一个肝脏占位的,结果是无原因的巨大血肿!
138
………
92
#B超#
31
概率有多大?
85
学习!
73