Lancet oncol:VR-CAP疗法相比R-CHOP可显著延长套细胞淋巴瘤患者的总体存活期
2018-10-29 MedSci MedSci原创
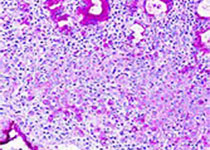
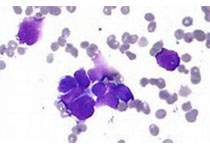
LYM-3002研究,在不适合进行移植的未治疗过的新确诊的套细胞淋巴瘤患者中对比硼替佐米联合利妥昔单抗、环磷酰胺、阿霉素和强的松(VR-CAP)和利妥昔单抗、环磷酰胺、阿霉素、长春新碱和强的松(R-CHOP)两种一线疗法的疗效和安全性。现研究人员对达到主要的无进展存活期结点后,长期随访阶段患者的最终总体存活期和安全预后结果进行报告。LYM-3002是在28个国家的128个临床中心开展的一项随机化的
LYM-3002是在28个国家的128个临床中心开展的一项随机化的开放性的3期研究。招募确诊的II-IV期未治疗过的、不适合进行骨髓移植的套细胞淋巴瘤成年患者,ECOG状态评分≤2分,被随机(按1:1)分至VR-CAP组(静滴 利妥昔单抗 375mg/m2、环磷酰胺 750mg/m2、阿霉素 50mg/m2和硼替佐米 1.3mg/m2,联合口服强的松100mg/m2)或R-CHOP组(静滴 长春新碱1.4mg/m2[最大剂量2mg]、利妥昔单抗 375mg/m2、环磷酰胺 750mg/m2和阿霉素 50mg/m2,联合口服强的松100m/m2),21天一疗程,6或8个疗程。本次分析的主要结点是总体存活期。
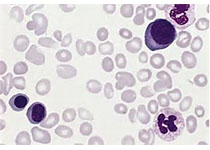
2008年5月22日-2011年12月5日,共招募了487位患者,其中268位(VR-CAP组140位、R-CHOP组128位)被纳入随访分析,随访截止2013年12月2日。中位随访82.0个月(IQR 74.1-94.2),VR-CAP组的中位总体存活期明显长于R-CHOP组(90.7个月[95% CI 71.4-未达到] vs 55.7个月[47.2-68.9];风险比0.66[95% CI 0.51-0.85];p=0.001)。随访期间出现3种新的副反应事件(两种各1例4期肺腺癌、VR-CAP组1例4期胃癌、R-CHOP组1例2期肺炎)。VR-CAP组243位患者死亡103位(42%),R-CHOP组244位患者死亡138位(57%),最常见的死因是病程进展。
与R-CHOP相比,VR-CAP疗法可明显延长患者存活期,而且安全性可接受。
Prof Tadeusz Robak,et al. Frontline bortezomib, rituximab, cyclophosphamide, doxorubicin, and prednisone (VR-CAP) versus rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) in transplantation-ineligible patients with newly diagnosed mantle cell lymphoma: final overall survival results of a randomised, open-label, phase 3 study.The Lancet Oncology. October 19,2018.https://doi.org/10.1016/S1470-2045(18)30685-5
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#细胞淋巴瘤#
38
#Oncol#
36
#Lancet#
34
#CAP#
43
#R-CHOP#
48
#存活期#
32