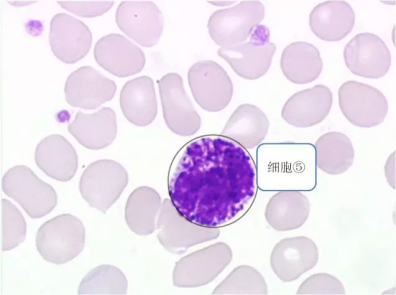
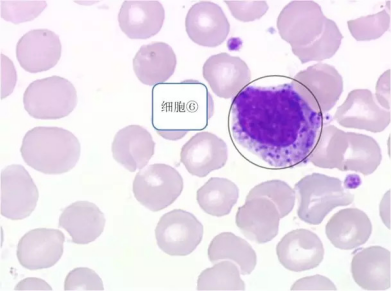
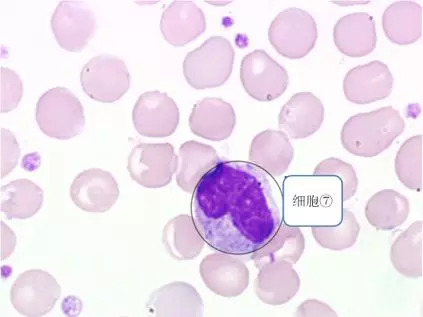
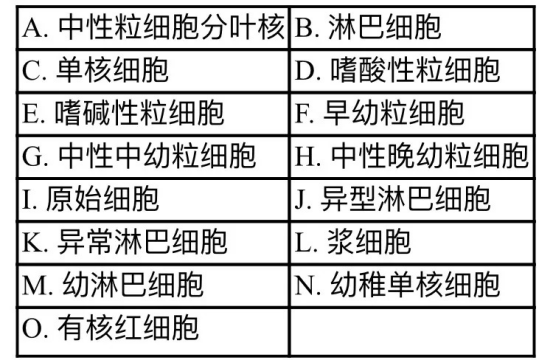
病例:这些特殊的白细胞你能认出几个?
2018-05-10 郭平(上海交通大学医学院附属瑞金医院检验科) 瑞金血液
这是来自瑞金血液的一份关于慢性粒细胞白血(chronic myelogenous leukemia,CML)的病例,查血常规时发现多种类型的白细胞,你能看图为白细胞分类吗?看看能得几分。





本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













学习了,谢谢作者分享!
63
好
75
好
0
学习.
77
学习了受益匪浅
77