干咳、活动后气短2年——闭塞性细支气管炎的诊断和治疗
2013-07-19 中国医学科学院 北京协和医院呼吸内科 柳涛 徐作军 中国医学论坛报
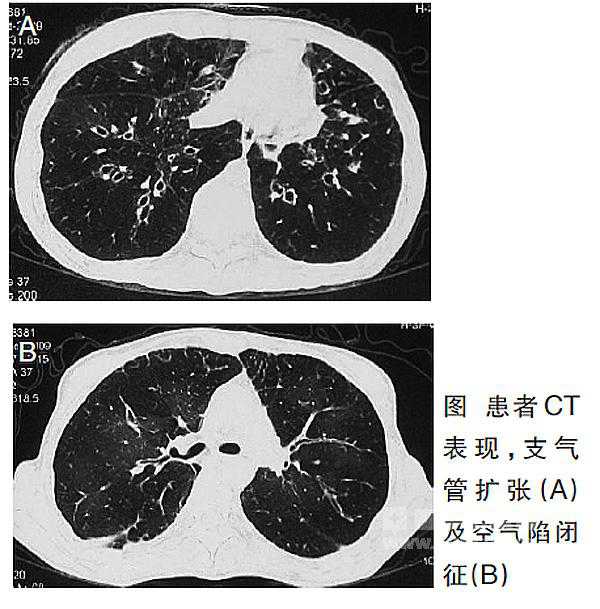
随着对造血干细胞移植(HSCT)后感染疾病的重视和积极治疗,非感染性并发症愈来愈多地呈现在我们眼前,且严重影响了患者预后。闭塞性细支气管炎(BO)是目前最常见的HSCT晚期肺非感染性并发症,症状多为干咳和呼吸困难,影像学可见空气陷闭征和支气管扩张等表现。BO致残率、病死率高,如何早期诊断、治疗BO对临床工作意义重大。 病历摘要 患者,女性,29岁
随着对造血干细胞移植(HSCT)后感染疾病的重视和积极治疗,非感染性并发症愈来愈多地呈现在我们眼前,且严重影响了患者预后。闭塞性细支气管炎(BO)是目前最常见的HSCT晚期肺非感染性并发症,症状多为干咳和呼吸困难,影像学可见空气陷闭征和支气管扩张等表现。BO致残率、病死率高,如何早期诊断、治疗BO对临床工作意义重大。
病历摘要
患者,女性,29岁。主因“进行性干咳、活动后气短2年”于2009年10月入院。
2007年11月,患者出现干咳、活动后气短,于当地医院就诊。肺功能检查提示,阻塞性通气功能障碍[1秒钟用力呼气容积(FEV1)为28.6%, FEV1/用力肺活量(FVC)为39.43%],长期口服阿奇霉素(250 mg qd)无效,干咳、呼吸困难进行性加重,活动耐量明显下降。
入院时查体 体重30 kg,半卧位,吸气三凹征明显,周身皮肤色素沉着,双肺呼吸音低,偶可闻及呼气相哮鸣音。
辅助检查 自然状态下动脉血气为,pH=7.386,动脉氧分压(PaO2)为46.2 mmHg,动脉二氧化碳分压(PaCO2)为45.8 mmHg,碳酸氢根(HCO3-)为26.9 mmol/L。
吸呼相胸部高分辨率CT(HRCT,下图)示,双肺中下叶支气管扩张,右侧少量气胸,空气陷闭征明显。
病毒、细菌、真菌相关检查,未见明显异常。
既往史 患者于2006年6月被诊断为急性粒细胞白血病M2型,4程化疗后完全缓解。2006年12月,接受马利兰预处理后行异基因造血干细胞移植。供者为其胞姐,配型全相合。移植后患者规律服用环孢素A(CsA,初为300 mg qd;逐渐减量至入院时25 mg qd),间断服用泼尼松。
2007年6月,患者出现口腔溃疡、躯干散在皮疹、腹泻,被诊断为移植物抗宿主病(GVHD),接受甲泼尼龙治疗后皮疹、腹泻好转,仍间断有口腔溃疡,伴口眼干。
诊断及治疗 结合临床症状、影像学检查,临床诊断为慢性GVHD,BO。
加用甲泼尼龙36 mg qd[泼尼松1.5 mg/(kg·d)],停用CsA,更换为他克莫司2 mg bid;口服阿奇霉素250 mg qd,每周5日;多潘立酮及埃索美拉唑镁肠溶片抗胃食管反流,复方异丙托溴铵、布地奈德雾化。患者呼吸困难症状有所改善。
讨论
BO是HSCT晚期常见的肺非感染性并发症,由于缺乏统一诊断标准,不同文献中HSCT后BO发生率约为0%~48%。国际骨髓移植登记处 (IBMTR)数据表明,在供者均为配型相合同胞的6275例HSCT患者中,1.7%于2年内发生BO。
闭塞性细支气管炎的病因及诊断标准
病因 HSCT后发生BO的确定因素包括异基因HSCT和慢性进展性GVHD。BO多发生在异基因移植,自体HSCT几乎不会发生;单独急性GVHD并不显著增加BO的发生风险。
发生BO的可能危险因素包括,新出现的或慢性隐匿性GVHD、受者年龄大、HSCT前存在气流阻塞(AFO,FEV1/FVC<70%)以及移植后早期呼吸道病毒感染。
发生BO的其他可疑因素包括,移植前马利兰预处理、供者配型非全相合或无关供者、低免疫球蛋白血症(特别是IgG和IgA)、应用甲氨蝶呤预防GVHD,原发病为慢性粒细胞性白血病(CML)、供者女性受者男性、既往有间质性肺炎、曾有中至重度急性GVHD以及全身放射治疗等。
本例患者为异基因移植且合并出现慢性GVHD,并经过马利兰预处理。
诊断标准 美国国立卫生研究院(NIH)于2005年提出,BO是唯一可以诊断慢性GVHD肺受累的肺部表现,并提出BO的诊断标准为,① AFO,即FEV1/FVC<70%,FEV1占预计值<75%;② 吸呼相HRCT可见空气陷闭征、小气道壁增厚或支气管扩张,肺功能残气量占预计值>120%,或病理学证实阻塞性细支气管炎;③ 根据临床表现、影像学和病原学检查可除外感染。
此外,非感染造成的闭塞性细支气管炎伴机化性肺炎(BOOP)也可见于急性或慢性GVHD。
闭塞性细支气管炎的症状与体征
症状 尽管有报告移植后30日内出现BO的病例,但BO主要于移植100天后出现(80%患者于移植后6~12个月起病)。本例患者于移植后11个月出现呼吸系统问题。
BO起病通常较为隐匿,临床症状无特异性,易误诊。23%的患者有前驱上呼吸道症状,主要表现为干咳(60%~100%)和呼吸困难(50%~70%),还可见喘息、鼻窦炎等。发热在无合并感染时少见。20%的患者可无明显临床症状,仅表现为肺功能异常。
体征 BO体征主要是小气道阻塞性病变相关症状,包括肺过度充气体征、呼吸音减弱、以及呼气相哮鸣音和高调的吸气中期干鸣音,肺底爆裂音少见。
BO患者几乎可以伴随存在慢性GVHD的任何症状和体征,特别是皮肤改变和口眼干。本例患者皮肤改变、口腔反复多发溃疡、口眼干。
胸部影像 BO早期的胸部影像学表现多数正常,晚期可见过度充气、支气管扩张及空气陷闭征。若出现气胸、纵隔气肿、心包积气等,提示预后差。
呼气相空气陷闭征对BO有高度提示意义,诊断BO的敏感性和特异性分别为74%~91%和67%~94%。研究表明,呼气相空气陷闭征在诊断BO上优于肺功能。
评估及随访BO变化时,推荐行吸呼相HRCT。
肺功能表现 BO患者肺功能表现为AFO,FEV1和FEV1/FVC降低,目前尚无统一诊断标准。支气管镜对诊断HSCT后BO意义较小,不推荐行经支气管镜肺活检(TBLB)。TBLB主要应用于除外感染性疾病。
闭塞性细支气管炎的治疗与转归
治疗 目前尚无治疗BO的规范化指南,治疗方案多基于小规模非对照临床研究及专家经验。BO的治疗与慢性GVHD相似,主要包括高剂量糖皮质激素和免疫抑制剂。
对症支持治疗在BO的治疗中占重要地位,其中包括气道支气管扩张剂的应用。
免疫抑制治疗前须通过临床、影像学、血清学和微生物学检查除外感染。开始免疫抑制剂治疗后,应予预防卡氏肺孢子菌肺炎(PCP),高危患者还应考虑预防性抗真菌和抗巨细胞病毒(CMV)。一旦出现感染应及时诊治。
终末期患者可考虑肺移植。有报告9例HSCT后BO患者行肺移植,其中5例行单侧肺移植、4例双侧肺移植,移植后随访9~72个月显示,3例因BO复发、慢性排异反应或感染死亡,其余未再出现BO表现 。
转归 HSCT后BO多呈慢性进展性病程,多数患者出现不可逆AFO,积极治疗仅有8%~20%患者肺功能可得到改善。绝大多数患者出现呼吸衰竭,部分因反复细菌感染出现支气管扩张。死亡率为14%~100%,平均65%,多数死于肺部感染。
本例患者因严重呼吸困难,生活不能完全自理。
随着移植技术的进步和临床广泛应用,以及急性GVHD和术后感染的进一步控制,我们在临床工作中将会遇到更多的BO患者,需要我们今后在临床和基础工作中重视BO,明确发病机理,寻求更好的预防治疗方法,减少患者痛苦。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








感谢分享一下!!!
62
#干咳#
38
#细支气管炎#
41
#细支气管#
38
#支气管#
40
#气短#
25