JACC:“Ross手术”可提高接受主动脉瓣置换术治疗患者的生存率
2022-02-28 “心关注”公众号 “心关注”公众号
美国纽约西奈山医院的研究人员首次将Ross手术与其他选择进行了比较,发现接受Ross 手术治疗的患者生存率不仅优于生物或机械主动脉瓣置换术,而且与匹配的美国普通人群相同。
主动脉瓣控制从心脏流入主动脉的血流,而主动脉是将血液输送到身体大部分部位的主要动脉。当瓣膜无法正常工作时,患者可能需要更换以保持心肌功能并防止心力衰竭或心源性猝死等问题。标准的心脏直视修复手术包括机械瓣膜置换术——使用人工制造的瓣膜,要求患者终身服用抗凝血剂以预防卒中,并进行一些生活方式的改变,例如避免可能导致跌倒和瘀伤的接触性运动;或来自人类或动物供体的生物主动脉瓣置换术,可能持续长达 20 年,但与机械瓣膜相比,年轻患者需要更早地再次手术。Ross手术是一种更复杂的手术,外科医生用患者自体肺动脉瓣替换主动脉瓣,这是正常主动脉瓣的镜像。这是Ross手术和生物或机械瓣膜置换术之间的根本区别,也是患者长期成功的关键因素。
近日,美国纽约西奈山医院的研究人员首次将Ross手术与其他选择进行了比较,发现接受Ross 手术治疗的患者生存率不仅优于生物或机械主动脉瓣置换术,而且与匹配的美国普通人群相同。因此,对于50岁以下患者的主动脉瓣置换术,Ross 手术可能比更标准的机械或生物置换术更有利。
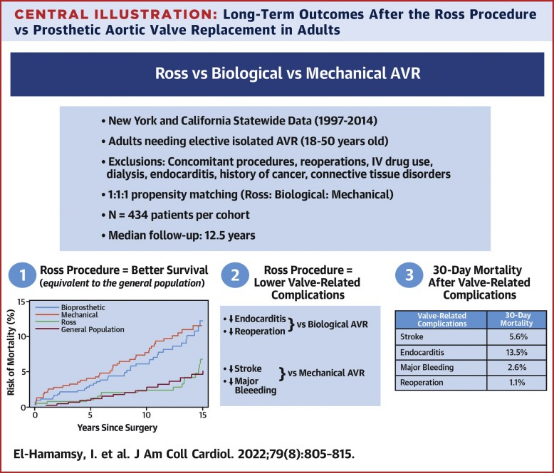
研究人员分析了 1997 年 1 月 1 日至 2014 年 12 月 31 日期间在加利福尼亚州和纽约州接受首次选择性主动脉瓣置换手术的 1,302 名 18 至 50 岁患者的记录。使用倾向匹配分析将患者平均分为三类,以消除任何基线差异:其中三分之一进行了Ross手术,三分之一进行了生物瓣膜置换术,其余进行了机械瓣膜置换术。这项回顾性研究比较了不同手术方式的长期生存率和瓣膜相关并发症(包括卒中、大出血、再手术和急性心内膜炎)的风险。
研究人员观察了受试者手术后 15 年的结果,发现接受Ross手术后患者的生存率明显提高。在 15 年时,与接受Ross手术治疗的患者相比,接受生物或机械主动脉瓣置换术的患者总死亡率高出两倍以上。此外,与未接受主动脉瓣置换手术的美国普通人群中同龄同性别的人相比,Ross 手术后的存活率(15 年时的存活率为 93%)是相同的。在瓣膜相关并发症方面,与机械瓣膜置换术相比,Ross 手术卒中或大出血的风险显着降低(Ross 手术后15年 3.8% vs. 机械瓣膜置换术后15年 13%)。同样,与生物瓣膜置换术相比,Ross 手术与再次手术(15年时17% vs. 30%)和心内膜炎(心脏组织感染)显着减少相关(15年时 2.3% vs. 15 年时的 8.5%)。然而,在 15 年时,Ross 手术后再次手术的风险高于机械瓣膜置换术(15年时17% vs. 7.4%)。
该研究还观察了发生任何瓣膜相关并发症(包括卒中、大出血、心内膜炎或再次手术)后 30 天的死亡率。研究人员发现,最低死亡率与再次手术有关(1%),而如果患者出现卒中、大出血或心内膜炎,相关死亡率至少高出三倍(卒中后为 5.6%,心内膜炎后为 13.5%)。
这项研究表明,虽然Ross手术后有一定的再次手术风险,但相关风险很低。换句话说,这应该被视为道路上的一个颠簸,而不是道路的尽头。相比之下,如果患者出现卒中、出血或感染,后果将更加可怕。研究人员表示,应该向患者提供所有这些数据,以便他们能够就这些重大生活事件做出真正明智的决定。总的来说,Ross手术与更好的生存和更少的并发症有关。
原始出处:
Ismail El-Hamamsy et al. Propensity-Matched Comparison of the Ross Procedure and Prosthetic Aortic Valve Replacement in Adults. Journal of American College of Cardiology, 2022,DOI: 10.1016/j.jacc.2021.11.057.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Ross手术#
47
#置换#
45
#JACC#
55
#生存率#
34
#ACC#
39
#主动脉瓣#
37
#ROS#
35
#主动脉瓣置换术#
42
#主动脉#
34
#置换术#
37