AMH值<0.5 ng/mL的女性流产风险高63%?
2023-09-11 生殖医学论坛 生殖医学论坛 发表于上海
以美国有商业保险的人群为研究对象,比较低AMH值(<0.5 ng/mL)和高AMH值(2.5–5.99 ng/mL和6–20 ng/mL)与正常AMH值(0.5–2.49 ng/mL)女性的流产风险。
美国生殖医学会(ASRM)年会是生殖医学领域规模最大、最具影响力的年度国际学术会议之一,覆盖生殖医学领域所有专业。2022年ASRM年会已经召开,生殖医学论坛精选了众多会议精华内容进行了翻译,希望给大家带来最新鲜、最前沿的生殖医学资讯。
本篇内容由翻译志愿者李维艳医生翻译,蔡贺博士审校,同时附上了原文,供大家学习交流!
Background
背景
The correlation between early pregnancy loss and maternal age is well-documented. As maternal age increases, anti-Mullerian hormone (AMH), a biomarker of ovarian reserve, decreases. There is evidence that AMH levels may be predictive of pregnancy outcomes independent of age. Low AMH values have been associated with increased risk of miscarriages , but data are conflicting and limited to analysis in specific populations, such as the infertile or older population. The relationship between high AMH and miscarriages is also unclear and limited by small sample sizes. A large cohort study in a more general population is necessary to understand this association and provide another counseling tool.
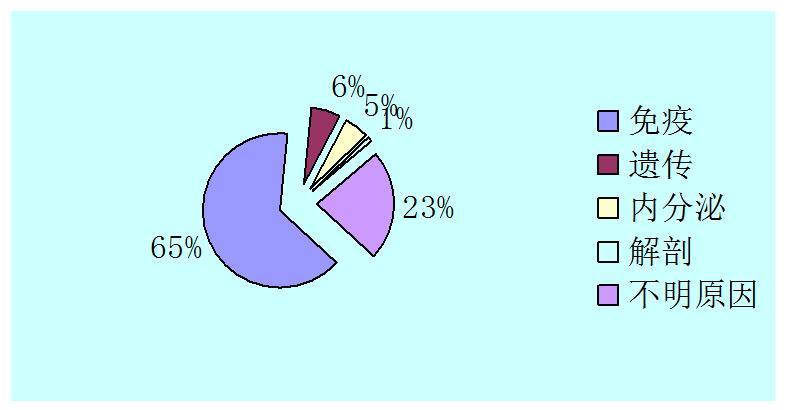
早期妊娠丢失与母体年龄之间的相关性已被充分证明。随着母体年龄的增加,作为卵巢储备生物标志物的抗苗勒氏激素(AMH)减少。有证据表明,AMH水平可以独立于年龄预测妊娠结局。低AMH值与流产风险增加相关,但因相关研究结果存在一定矛盾性,并且研究只限于某些特定人群,如不孕或高龄女性。高AMH与流产之间的关系也不确定且相关研究样本量均较少。因此一项针对一般人群的大样本队列研究对于了解AMH(高/低)与流产之间的关系以及提供相应咨询都是必要的。
Objective
目的
To compare risk of miscarriage in females with low AMH (<0.5 ng/mL) and high AMH (2.5–5.99 ng/mL and 6–20 ng/mL) levels with females with normal AMH values (0.5–2.49 ng/mL) in a general U.S. commercially insured population.
以美国有商业保险的人群为研究对象,比较低AMH值(<0.5 ng/mL)和高AMH值(2.5–5.99 ng/mL和6–20 ng/mL)与正常AMH值(0.5–2.49 ng/mL)女性的流产风险。
Materials and Methods
材料和方法
We used OptumLabs® Data Warehouse, a longitudinal, real-world data asset with de-identified administrative claims data (7), between 1/1/2005 – 6/31/2019. Using a validated approach to identifying pregnancy episodes, outcomes, and start dates in an administrative dataset using ICD, CPT, HCPCS, and LOINC codes (8), we restricted to pregnancies resulting in a live birth or a miscarriage with a start date no more than six months after an AMH test was performed. Females with cancer were excluded. Multivariable linear regression analyses were performed to assess the impact of AMH on the risk of spontaneous miscarriage adjusting for race, age, smoking, and obesity while also testing for interaction between age and AMH categories. Measures of association were expressed in adjusted risk ratios (aRR) and 95% confidence intervals.
选取2005年1月1日至2019年6月31日参保女性,应用了OptumLabs 数据库,该数据库包含的是一种纵向、真实世界的数据资料,也包含未识别的索赔数据管理。通过使用ICD、CPT、HCPCS和LOINC码在管理数据集中检索AMH检测后6个月内活产或流产的妊娠女性。排除恶性肿瘤女性。应用多变量线性回归分析,评估AMH对自然流产风险的影响,调整种族、年龄、吸烟和肥胖等因素,同时评价年龄和三类AMH(低值、高值、正常值)之间的交互作用。相关结果以调整后的风险比(aRR)和95%置信区间(CI)表示。
Results
结果
We identified 10,708 females who had AMH testing performed shortly before a pregnancy that would result in either a live birth or a miscarriage. There were 11,057 live births and 456 miscarriages identified. The geometric mean AMH among females who had a miscarriage was 1.45 ng/mL (95% CI: 1.22, 1.71) compared to the mean AMH among females with a live birth (2.16 ng/mL, 95% CI: 2.11, 2.22). In adjusted analysis, females with an AMH value less than 0.5 ng/mL were at 63% higher risk of experiencing a miscarriage (aRR 1.63, 95% CI: 1.22-2.17) compared to females with AMH values between 0.5 and 2.49 ng/mL. There were no differences in risk of miscarriage in females with AMH values between 2.5 and 5.99 ng/mL (aRR 0.94, 95% CI 0.75-1.18) or between 6 and 20 ng/mL (aRR 0.93, 95% CI: 0.69-1.24) compared to the reference group. Interaction terms between age and AMH were not significant.
纳入的10708名女性在妊娠前不久进行了AMH检测,其中11057例活产和456例流产。流产和活产女性AMH的几何均数分别为1.45ng/mL(95%CI:1.22,1.71)和2.16ng/mL(95%CI:2.11,2.22)。AMH值小于0.5 ng/mL(低AMH)的女性流产风险比正常AMH值(0.5–2.49 ng/mL)的女性高63%(aRR 1.63,95%CI:1.22-2.17);AMH值在2.5–5.99 ng/mL和6–20 ng/mL的女性流产风险无差异(aRR 0.94,95%CI 0.75-1.18和aRR 0.93,95%可CI:0.69-1.24)。年龄与AMH之间的交互作用不显著。
Conclusions
结论
The use of an administrative dataset consisting of a large population further supports evidence that low AMH levels are related to more miscarriages. This association did not differ by age. This study demonstrates that low AMH is a marker of reduced fecundity in a more general population.
本研究应用大样本数据进一步支持了AMH水平低与流产相关,且二者的关联独立于年龄因素。该研究表明,在广泛的人群中,低AMH是生育力降低的标志。
文章来源:LOW ANTI-MULLERIAN HORMONE LEVELS ARE ASSOCIATED WITH MISCARRIAGE IN A GENERAL FEMALE POPULATION Zhou, Beth et al.Fertility and Sterility, Volume 118, Issue 5, e20
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













好
34