Mol. Cell:启动癌细胞对糖嗜好的丙酮酸脱氢酶激酶或为抗癌靶标
2012-01-06 MedSci MedSci原创
癌细胞对糖的渴望,部分上是因为它们关闭它们的线粒体——能够有效燃烧葡萄糖的动力厂——以便偏好一种更加无效率的方式使用葡萄糖。它们获益,因为副产物能够为快速生长的癌细胞提供构建材料。 美国埃默里大学温希普癌症研究所科学家证实很多类型的癌细胞扳动开关让葡萄糖从线粒体转移走。他们的发现提示着促进几种类型癌症生长的酪氨酸激酶在线粒体中发挥的作用要比人们以前所认识的大得多。 这些结果也突出地显示丙酮
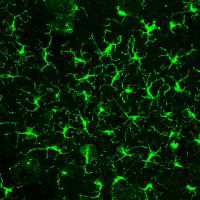
癌细胞对糖的渴望,部分上是因为它们关闭它们的线粒体——能够有效燃烧葡萄糖的动力厂——以便偏好一种更加无效率的方式使用葡萄糖。它们获益,因为副产物能够为快速生长的癌细胞提供构建材料。 美国埃默里大学温希普癌症研究所科学家证实很多类型的癌细胞扳动开关让葡萄糖从线粒体转移走。他们的发现提示着促进几种类型癌症生长的酪氨酸激酶在线粒体中发挥的作用要比人们以前所认识的大得多。 这些结果也突出地显示丙酮酸脱氢酶激酶(pyruvate dehydrogenase kinase, PDHK)在控制癌细胞代谢中发挥着重要作用。2011年12月21日,该研究在线发表在《分子细胞》(Molecular Cell)期刊上。 埃默里大学温希普癌症研究所血液学和医学肿瘤学副教授Jing Chen说,“我们和其他人已证实PDHK在人几种类型癌症中上调表达,但是我们发现在癌细胞中存在一种增强PDHK活性的新方法。基于PDHK在调节癌细胞代谢上的作用,PDHK对于抗癌治疗而言是一个非常吸引人的靶标。” Chen和埃默里大学医学院血液学和医学肿瘤学副教授Sumin Kang博士是这篇研究的共同通讯作者。博士后青年Taro
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Cell#
29
#CEL#
23
#癌细胞#
24
#靶标#
42
#激酶#
31