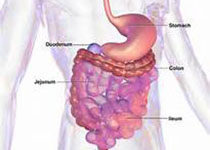
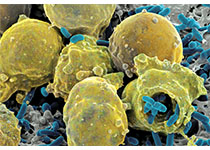
Nat Microbiol:科学家为肠道细菌编写分子食谱
2018-04-05 佚名 中国生物技术网
科学家们编写了一本不同寻常的食谱,不仅适用于我们人类,而且是专门为我们体内的微生物写的。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CRO#
22
#Nat#
28
#Bio#
25
#Biol#
29
#Micro#
28
每日必看
0
#肠道细菌#
26
学习了
62
肠道细菌研究热点
62
vv黄河鬼棺哈哈
50