JAMA Netw Open:晚期口咽鳞状细胞癌的更佳初始治疗方案?
2021-06-04 Nebula MedSci原创
针对性放化疗和前期手术治疗都被认为是晚期口咽鳞状细胞癌的标准方案。但哪一个是最佳治疗方式仍不明确
针对性放化疗(Definitive chemoradiotherapy)和前期手术治疗(Upfront surgical treatment)都被认为是晚期口咽鳞状细胞癌的标准方案。但是,晚期口咽鳞状细胞癌的最佳主要治疗方式仍不明确。
该研究旨在对比晚期口咽鳞状细胞癌采用针对性放化疗和前期手术治疗的疗效。
这是一项回顾性的疗效对比分析,纳入了2007年至2015年确诊的III期或IV期口咽鳞状细胞癌(排除T4b或N3期的患者);于2019年6月至2020年12月进行数据分析。主要终点是总生存率。次要终点是无进展生存期、无局部复发生存期和无远处转移生存期。
共招募了1180例患者(89.1%的男性,平均54.59岁):针对性放化疗组 694例(58.8%),前期手术治疗组 486例(41.2%)。大部分患者为扁桃体原发肿瘤(712例[60.3%])、中级分化组织学(604例[51.2%])、临床N2期(858例[72.7%])、临床分期IVA疾病期(938例)。
两组患者的总生存率
中位随访了3.62年(四分位数范围:1.63-5.47)。以前期手术治疗为主要治疗方式与研究期间患者的死亡风险降低相关(风险比[HR] 0.81; 95% CI, 0.69-0.97; P=0.02)。但是,根据年龄、部位、组织学等级和T/N分组后,前期手术治疗不再与研究期间患者的死亡风险降低相关(HR 0.96; 95% CI, 0.80-1.16; P=0.70)。
两组患者的无进展生存期
前期手术治疗组的无进展生存期较针对性放化疗组的差(HR 1.64; 95% CI, 1.09-2.46; P=0.02),而且,根据其他预后相关因素校准后,这种差异仍然存在(如年龄、肿瘤部位等)(HR 1.72; 95% CI, 1.12-2.66; P=0.01)。
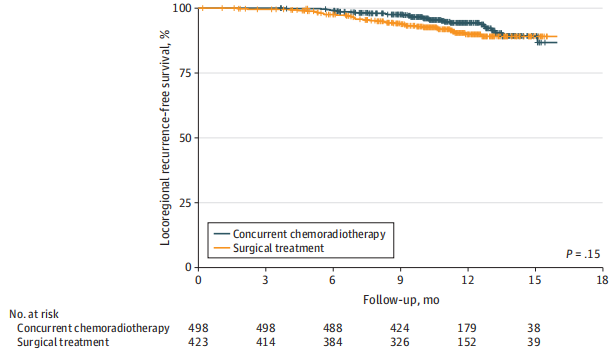
两组患者的无局部复发生存期
综上所述,该研究结果显示,根据预后相关的基线因素校准后,针对性放化疗的疗效可与前期手术治疗的相媲美。总而言之,在该研究中,针对性放化疗和前期手术治疗在晚期口咽鳞状细胞癌中的疗效仍不分伯仲。
原始出处:
Tsai Mu-Hung,Cheng Yung-Jen,Pao Tzu-Hui et al. Association of Primary Treatment Modality for Advanced-Stage Oropharyngeal Squamous Cell Carcinoma With Survival Outcomes.[J] .JAMA Netw Open, 2021, 4: e2112067.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#NET#
35
#细胞癌#
43
#PE#
34
#治疗方案#
31
#初始治疗#
43
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
46