Front Oncol:AFP早期应答与仑伐替尼治疗HBV相关肝细胞癌生存相关
2022-03-02 yd2015 MedSci原创
研究表明,AFP早期应答是仑伐替尼治疗HBV相关肝细胞癌生存相关的预后因素。
Lenvatinib(仑伐替尼)是不可切除的肝细胞癌(uHCC)的一线治疗药物。近期,来自吉林大学第一附属医院的团队开展了相关研究,主要是评估早期甲胎蛋白(AFP)应答对预测仑伐替尼治疗HBV相关uHCC的临床预后作用。相关结果发表在Frontiers in Oncology杂志上。

这项回顾性分析纳入2018年11月-2021年5月期间接受仑伐替尼治疗>1个月的HBV相关uHCC和AFP基线水平>20 ng/ml的患者。早期AFP应答定义为lenvatinib治疗4周后AFP血清水平较基线下降>20%。对AFP反应者和无反应者进行放射学应答(实体肿瘤反应评价标准v1.1)、无进展生存期和总生存期评估。
研究筛查79例患者,最终纳入46例患者。基线时,超过一半的患者(65.2%)为Child-Pugh A级。52.2%的患者有肝外转移,34.8%的患者有门静脉血栓形成。中位肿瘤大小为5.6 cm, 17.4%和80.4%的患者分别为BCLC-B期和C期。总的来说,82.6%的患者接受了lenvatinib作为一线治疗。作为二线治疗的患者均是在索拉非尼治疗进展后使用。中位随访期18.0个月(IQR, 3-29个月)。总的来说,10例(21.7%)患者lenvatinib剂量减少,3例(6.5%)患者因AEs而中断治疗。
46例患者中,30例(65.2%)为早期AFP应答者,16例(34.8%)为无反应者。早期AFP应答者和无反应者的中位基线AFP水平分别为660.25 ng/ml和1199.0 ng/ml。除年龄(p=0.0336)、门静脉血栓形成(p=0.0205)和腹水(p=0.04)外,早期AFP应答者和无反应者的基线特征相似。
在早期AFP应答组中,PR、SD和PD分别为10例(34.5%)、14例(48.3%)和5例(17.2%),而无反应组分别为1例(6.3%)、7例(43.8%)和8例(50.0%)。早期AFP应答组的ORR(34.5% vs 6.3%;p=0.0349)和DCR (82.8% vs 50.0%;p = 0.0203)较无应答组明显增高。

早期AFP应答者的中位无进展生存期(PFS)明显长于无应答者(13.0 vs 7.0个月;p = 0.028);早期AFP反应者的中位OS为17.0个月,而无反应者的中位OS为12.0个月,两组没有统计学差异(p=0.16)。
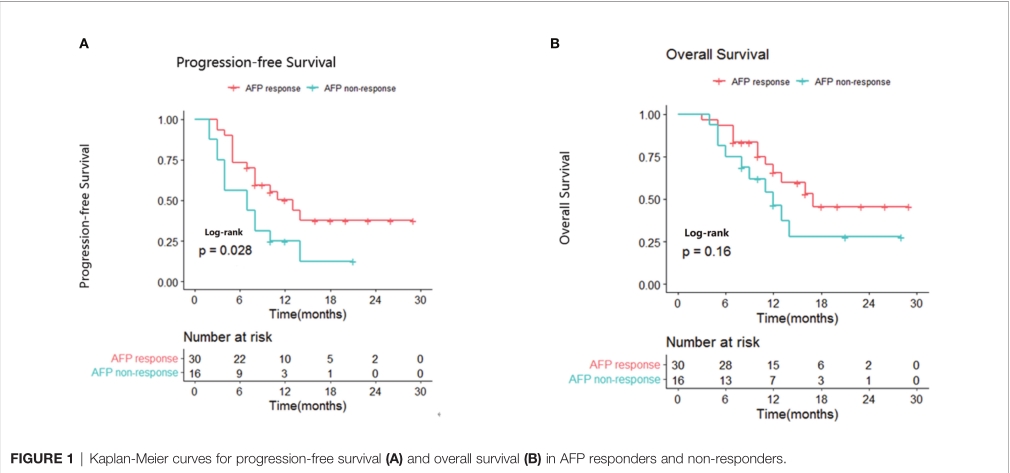
在单因素分析中,有可能获得更长的无进展生存期的因素有:早期AFP应答者(HR, 0.464;95%CI,0.222 -0.967;p=0.0404), ECOG PS为0 (HR, 0.431;95%CI 0.265-0.897;p=0.0398)和ALBI 1级(HR, 0.538;95%CI,0.290 - 0.973;p = 0.0462)。随后的多因素分析证实早期AFP应答者(HR, 0.387;95%CI,0.183-0.992;p=0.0154),ECOG PS为0 (HR, 0.890;95%置信区间,0.811-0.976;p=0.0132)和ALBI 1级(HR, 0.457;95%CI,0.269-0.963;P =0.0327)是PFS的独立良好预后因素。

在单因素分析中,有可能获得更长的OS的因素有:ECOG PS为0 (HR, 0.531;95%CI,0.324-0.991;p=0.0498)和ALBI 1级(HR, 0.434;95%CI 0.258-0.855;p = 0.0320)。多因素分析显示,ECOG PS为0 (HR, 0.479;95%CI,0.314 - 0.876;p=0.0332), ALBI 1级(HR, 0.551;95%CI,0.160 -0.897;p=0.0346)是延长OS的独立预后因素。

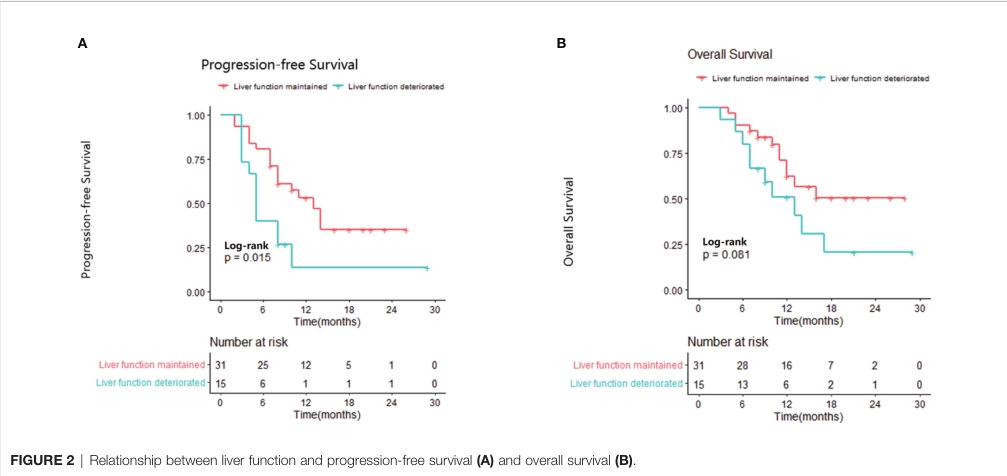
与那些在治疗期间肝功能恶化的患者相比,肝功能保持或改善的患者的中位PFS显著延长(13.0个月vs 5.0个月;p = 0.015)。维持或改善的肝功能组的中位OS未达到,肝功能恶化组的中位OS为13个月(p=0.081)。
综上,研究表明,AFP早期应答是仑伐替尼治疗HBV相关肝细胞癌生存相关的预后因素。
原始出处:
Liu B, Shang X, Shi J-Y, Cui G-Z, Li X and Wang N-Y (2022) Early Alpha-Fetoprotein Response Is Associated With Survival in Patients With HBV-Related Hepatocellular Carcinoma Receiving Lenvatinib. Front. Oncol. 12:807189.doi: 10.3389/fonc.2022.807189.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#HBV#
57
#肝细胞#
31
#Oncol#
34
#细胞癌#
29
#AFP#
44
学习了
57