67岁,男性,因为左侧上肢无力1h就诊。
NIHSS 2分,拒绝静脉溶栓。
既往史:高血压和高脂血症。
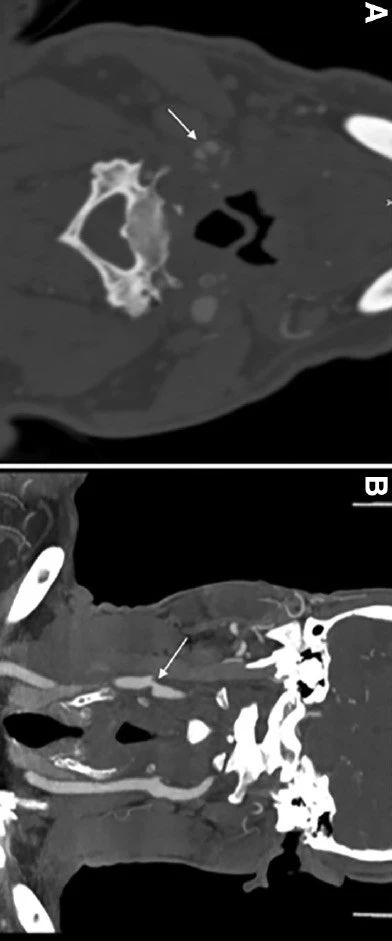
头颈 CTA 显示右侧颈内动脉后壁发出层状充盈缺损,伴30-50%狭窄。轴位 CTA 证实为腔内隔膜,符合颈动脉蹼的表现,无钙化,也没有附着的血栓(下图):
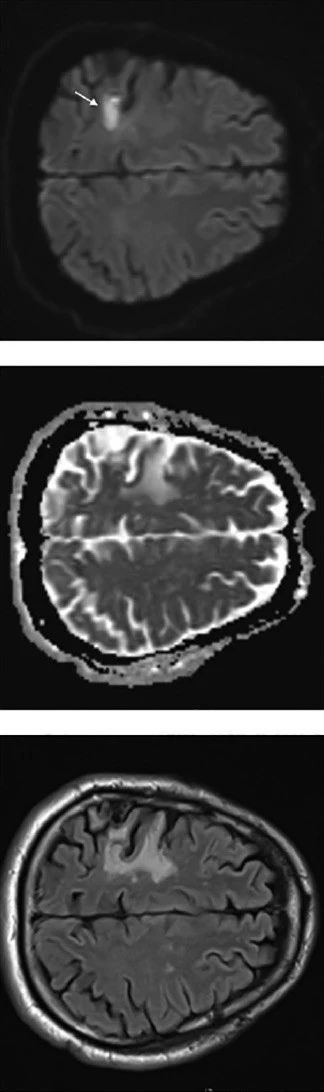
脑MRI 显示右侧额叶急性梗死,累及右侧运动皮层(下图),同时可见同一动脉供血区陈旧性脑栓塞性梗死:
对侧颈内动脉、颅内动脉未见动脉闭塞、狭窄或严重异常。经胸超声和心电监测未见异常。心电图监测未见房颤。
开始给予阿司匹林100mg,每天一次。11个月后再发左侧面部下垂,左上肢无力和构音障碍。
头 MRI 显示上一次梗死灶旁新发梗死(下图):
脑CTA显示右侧 MCA M2段新发闭塞。颈部 CTA 显示右侧颈内动脉狭窄,狭窄程度和腔内病变的形态与前一次相比没有变化。
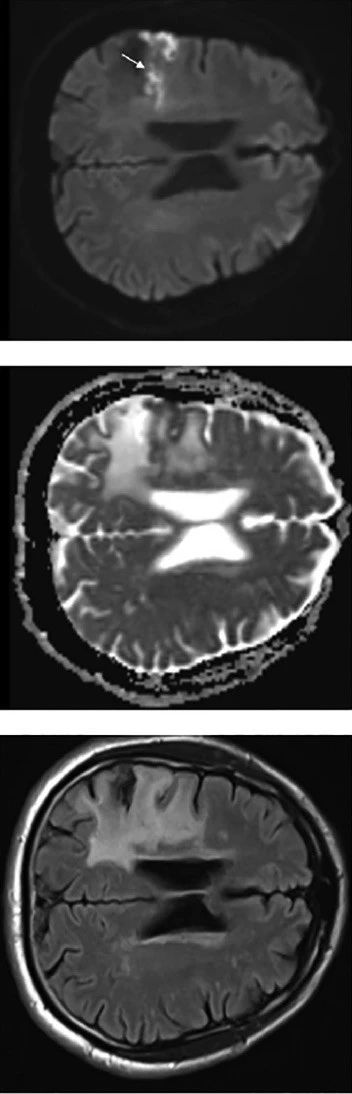
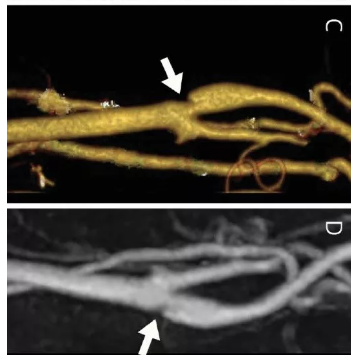
DSA 进一步证实为颈动脉蹼,患者随后进行了血管内治疗,右侧颈内动脉置入自膨支架,治疗后狭窄明显好转:
患者症状完全缓解,出院给予双抗治疗3个月,以后长期阿司匹林单抗治疗。
原始出处:Brian Mac Grory , Derrick Cheng , Curt Doberstein , et al. Ischemic Stroke and Internal Carotid Artery Web: A Case Study. Stroke. 9 Jan 2019
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#颈动脉#
27
#成形术#
34
#颈动脉蹼#
41
不错
68