Antimicrob Agents Chemother:广泛耐药肺结核:氯法齐明获益有限!
2018-08-15 吴星 环球医学
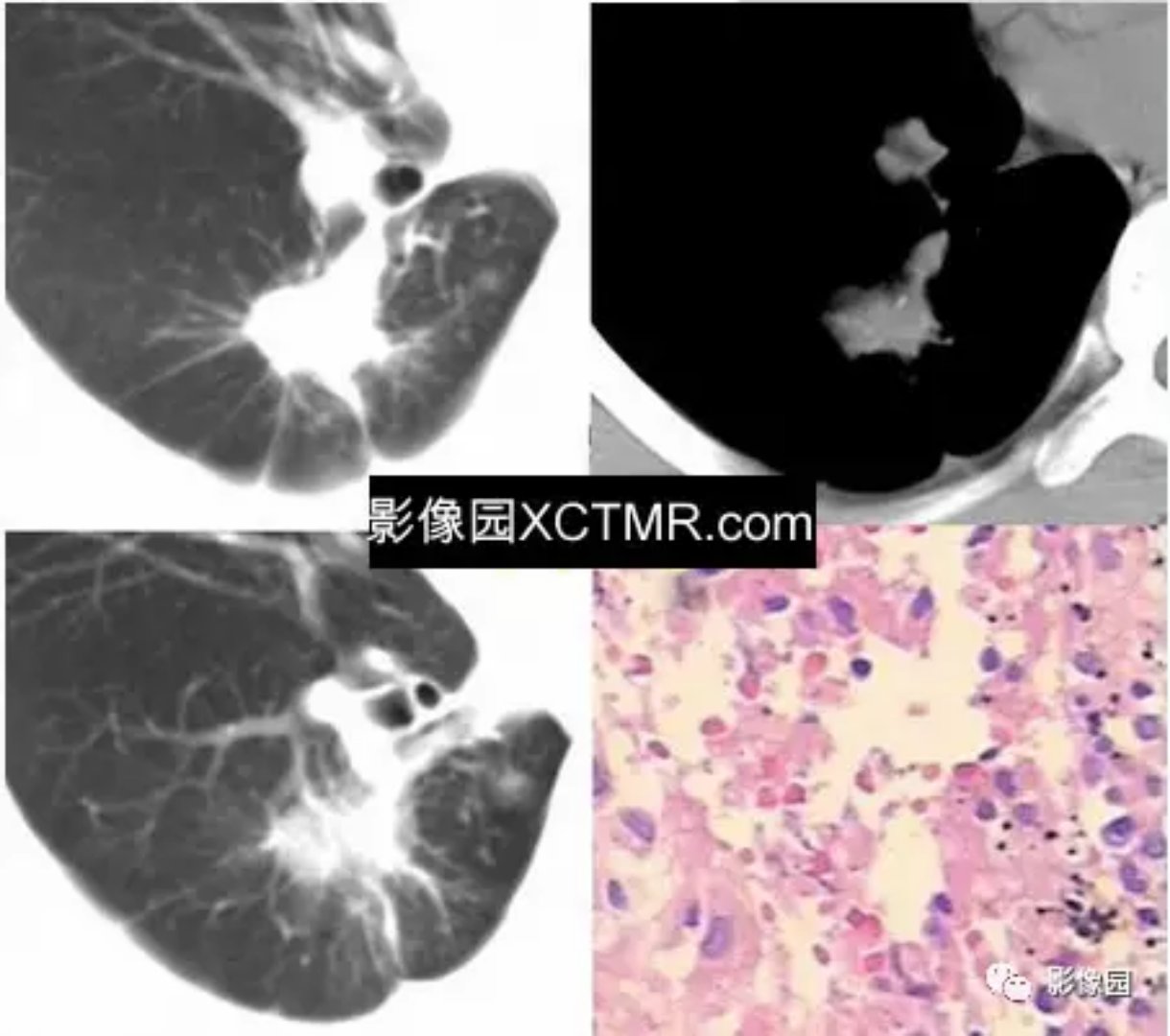
由于耐药结核病的诊断复杂,治疗困难,对个人、家庭及社会均造成巨大的经济压力。2018年3月,发表在《Antimicrob Agents Chemother》的一项多中心、前瞻性、随机研究,旨在调查在中国氯法齐明(CLO)治疗广泛耐药肺结核(XDR-TB)的有效性和安全性。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Agent#
38
#CRO#
31
#agents#
35
#Micro#
23
#结核#
33
#氯法齐明#
45
好文,值得点赞!认真学习了,把经验应用于实践,为患者解除病痛。
57