再次活检明确小细胞肺癌:全身治疗 or 局部治疗?
2017-11-19 佚名 肿瘤资讯
在第一期的MDT中我们讨论了一例PET/CT提示肺癌多发转移,但多次活检未获得恶性肿瘤证据的病例。经过激烈的讨论制定了下一步的诊疗计划:先进行支气管镜检查。那么,在一周后,该病例的诊断有什么进展?又该如何选择下一步的治疗方案?
在第一期的MDT中我们讨论了一例PET/CT提示肺癌多发转移,但多次活检未获得恶性肿瘤证据的病例。经过激烈的讨论制定了下一步的诊疗计划:先进行支气管镜检查。那么,在一周后,该病例的诊断有什么进展?又该如何选择下一步的治疗方案?
吴一龙(教授、主任医师、博导)、张绪超(研究员、硕导)、杨衿记(主任医师、博导)、杨学宁(主任医师)、钟文昭(主任医师、博导)、周清(主任医师、博导)、涂海燕(副主任医师)、陈晓明(主任医师、硕导)、李伟雄(主任医师)、潘燚(副主任医师)、陈华军(副主任医师)、汪斌超(副主任医师)、王震(副主任医师)、徐崇锐(主治医师)、廖日强(主治医师)、董嵩(主治医师)、江本元(医师)、白晓燕(医师)、孙月丽(医师)、陈志勇(医师)、李安娜(医师)、郑明英(医师)、林嘉欣(医师)、白晓燕(医师)、林辉(医师)、黄婕(医师);全体在读研究生。
病例汇报人:广东省人民医院肺一科 彭晓潇医师
患者病史
1. 58岁男性,重度吸烟者,已戒烟4年。
2. 主诉:咳嗽、咳血丝痰1月余。无发热、乏力、盗汗。
3. 重度吸烟史,已戒烟4年。
4. 无肿瘤家族史。
5. 外院CT示右肺占位。
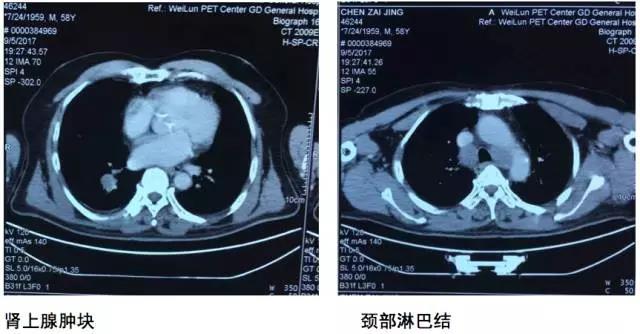
6. 2017-9-5广东省人民医院PET提示:右肺下叶肿物2.8*2.7cm,SUV 22.3,双侧颈部、双侧气管旁、隆突下、食管旁、右侧肺门淋巴结肿大,代谢升高,考虑为转移灶,右侧肾上腺转移灶,具体结果见下图:


CA19-9(电发光法):7.35 U/ml; 非小细胞肺癌相关抗原(电发光法):1.76 ng/ml;AFP(发光法):1.89 ng/ml; CEA(发光法):2.30 ng/ml。
拟行肺穿刺CT:

上周MDT讨论意见:完善纤维支气管镜检查,若找到恶性肿瘤证据,按标准方案治疗;若仍无恶性肿瘤证据,再次讨论。
本周更新:
2017-09-26纤维支气管镜活检:
镜下见:气管管腔通畅,黏膜光滑,未见狭窄、新生物及出血。右下叶外基底支B9可见新生物,黏膜充血,触之易出血,其余左右主支气管及各叶段支气管管腔通畅,黏膜光滑,分泌物不多,未见狭窄、新生物及出血。
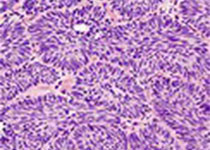
病理结果示:小细胞癌。
病史小结
最终诊断:右肺下叶小细胞癌cT1cN0M1b IVA期(肾上腺)(8th)
病例讨论
肺内科周清医生:在上周的讨论中我们提到,PET高度怀疑是肺癌伴肾上腺、淋巴结转移,同时也与PET室教授沟通,即便病理阴性,他们仍然认为根据影像学表现,是恶性疾病。当时已经对两处病灶进行活检,均为阴性,上周讨论时出现两个观点:一派认为可以先观察两个月,还有一派认为要想办法再取活检,如何取活检也有两个意见,一个是通过气管镜取,因为患者有咳血,另外一个意见认为对肾上腺病灶进行手术。现在回过头来看,我认为从这个患病例中我们吸取一个经验:因为该患者影像学有支持恶性肿瘤的特征,有咳血的症状,同时与小细胞肺癌相关的肿瘤标志物NSE升高,这些都与患者肺癌的诊断符合。因此当遇到此类病例,当有证据支持恶性肿瘤时,我们不能轻易的考虑用风湿免疫疾病解释,而是尽量的查找肿瘤或者考虑肿瘤合并其它炎症性淋巴结存在的可能性。从我们肿瘤科的角度,最怕的就是漏诊,最怕现在说不是恶性肿瘤,过段时间发现是恶性,甚至广泛转移了。我们最不希望出现这种情况,因此能追根问底的尽量的去寻找病理诊断非常重要。
现在纤维气管镜发现小细胞肺癌的证据,但并代表所有的问题都解决了。根据患者影像学特征,小细胞肺癌的确有可能出现小病灶大转移,但是如果只是孤立肾上腺转移,没有淋巴结转移的情况相对少见。因此这些淋巴结究竟是良性的,还是因为取材有限,只是取到了良恶性混杂的良性部分?对于淋巴结N0的分期还是一个问号。我认为在现阶段不用再纠结是否再去取淋巴结,我们知道小细胞肺癌主要以化疗为主,我们可以在化疗后观察患者纵隔淋巴结和肾上腺病灶的变化,如果经济条件好可以考虑再次行PET检查,如果化疗后,淋巴结和肾上腺病灶的大小或者代谢都有改变,可能才会进一步明确患者的分期。
肺内科涂海燕医生:请问外科医生,我们在CT上看到的肿块和纤维支气管镜看到的右下叶外基底支B9开口处的肿块是同一个肿块吗?(是)另外对于淋巴结的肉芽肿性炎,我们医院只做了抗酸染色,是否有做T-SPOT等结核相关检查?因为小细胞肺癌要化疗,要明确患者是否有活动性的结核或者其他的感染,否则给予化疗可能会导致结核增殖。肉芽肿性炎只是我们看到的现象,希望尽量能找到病因,因此我认为还可以请风湿免疫科会诊,完善风湿免疫相关指标的检测,同时排除感染。
吴一龙医生:根据彭医生病例汇报中提到的诊断小细胞癌cT1cN0M1b IVA期,目前对于淋巴结并没有恶性肿瘤的证据,因此患者分期N3是不成立的,目前的分期应该是T1N0M1a。目前对于小细胞肺癌的治疗,近十年来取得比较大的一个进展就是将外科治疗重新拉了回来。最开始认为小细胞肺癌需要手术治疗,上海市胸科医院吴善芳教授也是因为当年做小细胞肺癌的外科手术世界知名,但是后来又发现了小细胞肺癌手术治疗疗效不好,因此后面很长一段时间由内科医生统治了小细胞肺癌的治疗,那个阶段认为无论小细胞肺癌属于哪个分期,永远都是内科治疗。这个观点一直统治到我们高峰论坛小细胞肺癌专题那届,我们整理了所有的数据,得到了一个比较明确的共识:如果是早期小细胞肺癌外科手术的干预很重要,尤其是在没有纵隔淋巴结转移的情况下,应该用外科手术进行干预。我们的共识发表没多久时间,NCCN指南也同时提出对于非常早期的小细胞肺癌也应该考虑外科干预。除此之外,近年来其它的关于小细胞肺癌的进展就乏善可陈了。对于今天这个病例,与我们刚才讨论的略有不同:PET-CT中明确显示了纵隔淋巴结高代谢,尽管病理提示肉芽肿性炎,但是肉芽肿也可以表现为高代谢。
目前我们既然明确了小细胞肺癌的病理诊断,又怀疑肾上腺病灶等可能是转移。我们现在的问题就是:是选择先明确是否是转移然后进行外科干预,还是先给予化疗。对于这个病例有很多不确定的因素存在,我还是认为应该先进行全身治疗,但是我们一定要记住,局部治疗扮演非常重要的作用,包括手术和放疗。因此不要等4-6个周期化疗后再请我们局部治疗的医生,而是在大概一两个周期之后马上要请局部治疗的医生来讨论下一步的治疗方案。所以我们今天强调的是对于这个病例,全身治疗应该先行,但千万要记住局部治疗将扮演重要的角色,及早与外科和放疗科医生进行沟通。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#活检#
38
#局部#
43
#局部治疗#
57
学习了.谢谢分享.
91
学习一下谢谢
80
好资料学习了!
56