CLIN CANCER RES:Ricolinostat联合硼替佐米以及地塞米松治疗复发或难治性多发性骨髓瘤
2017-07-08 MedSci MedSci原创
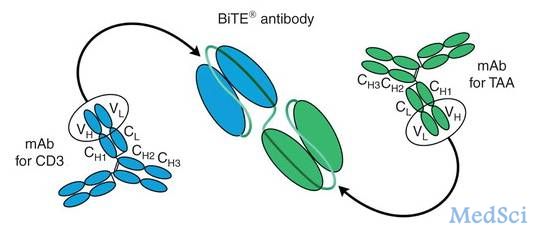
抑制组蛋白脱乙酰基酶(HDAC)可以增强蛋白酶体抑制作用治疗多发性骨髓瘤的疗效,但是也会增加毒性。临床前研究发现HDAC6通过蛋白质降解过程中的聚集体/自噬途径调节蛋白体酶抑制抵抗。CLIN CANCER RES近期发表了一篇文章,报道HDAC6选择性抑制剂Ricolinostat的临床试验结果。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#多发性#
41
学习一下吧!学习一下了
58
#难治性#
37
学习了谢谢分享
56
好文,值得点赞!认真学习了,把经验应用于实践,为患者解除病痛。
60
学习了谢谢分享
65
学习了,谢谢作者分享!
54