Thorax:从低剂量CT扫描和吸烟因素预测肺癌的可行性
2019-03-26 xiangting MedSci原创
LCCM具有作为肺癌预测因子的前途,因为它相对现有模型有显著的改善。
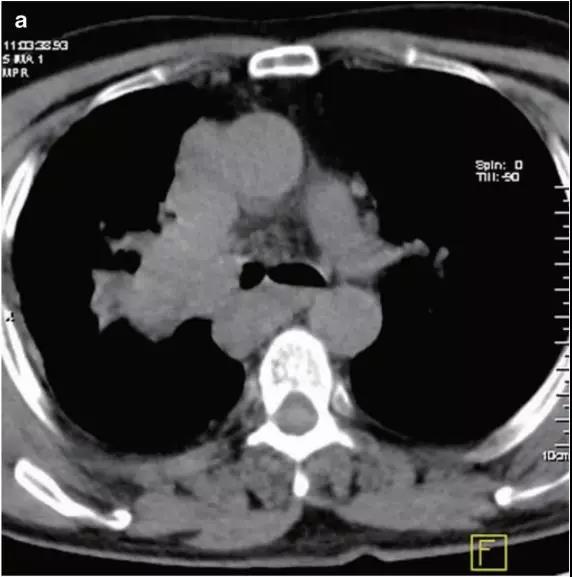
低剂量CT(LDCT)目前用于高危人群的肺癌筛查,以早期诊断肺癌。然而,96%检测到结节的个体是假阳性。
为了从临床、人口学和LDCT特征开发有效的早期肺癌预测因子,研究人员对218名肺癌或良性结节受试者进行了研究。使用概率图模型(PGMs)整合来自匹兹堡肺部筛查研究队列92名受试者(训练队列)的人口学、临床数据和LDCT特征。
学习后的PGMs确定了3个直接(因果)与恶性结节和最大良性结节相关的变量,并用它们构建了肺癌因果模型(LCCM),该模型在126名受试者的单独队列中得到验证。结节、血管数量和受试者戒烟年数足以区分恶性结节与良性结节。在训练和验证队列中与现有预测因子进行比较表明:(1)结合LDCT扫描特征大大提高了预测的准确性;(2)LCCM改善癌症检测优于现有的方法,包括Brock简约模型(p<0.001)。值得注意的是,周围血管数量,这个以前未在预测模型中使用的特征,显著提高了预测效率。根据验证队列结果,LCCM能够识别30%的良性结节,而没有错误分类癌结节的风险。
LCCM具有作为肺癌预测因子的前途,因为它相对现有模型有显著的改善。在更大的前瞻性研究中进行验证后,LCCM有助于减少不必要的随访和手术。
原始出处:
Vineet K Raghu. Feasibility of lung cancer prediction from low-dose CT scan and smoking factors using causal models. Thorax. 12 March 2019.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#可行性#
35
#低剂量CT#
48
#低剂量#
40
#CT扫描#
47