ASCO 2015:Palbociclib 改善乳腺癌PFS(PALOMA-3试验)
2015-05-29 佚名 中国医学论坛报今日肿瘤
PALOMA-3 Ⅲ期临床研究经独立小组分析显示达到其主要研究终点而被提前终止。该研究显示Palbociclib可显著改善HR+ / HER2- 乳腺癌患者">乳腺癌患者的无进展生存(PFS)期。这是首个报道的关于CDK 4 / 6抑制剂随机Ⅲ期临床的数据。多中心PALOMA-3研究随机入组521例转移性乳腺癌患者,这些患者在内分泌治疗进展后以2:1比例随机入组氟维司群(FASLODEX)+
PALOMA-3 Ⅲ期临床研究经独立小组分析显示达到其主要研究终点而被提前终止。该研究显示Palbociclib可显著改善HR+ / HER2- 乳腺癌患者">乳腺癌患者的无进展生存(PFS)期。这是首个报道的关于CDK 4 / 6抑制剂随机Ⅲ期临床的数据。多中心PALOMA-3研究随机入组521例转移性乳腺癌患者,这些患者在内分泌治疗进展后以2:1比例随机入组氟维司群(FASLODEX)+安慰剂(对照组)或氟维司群+palbociclib(治疗组)对其疗效进行评估。FASLODEX 首次给药500mg d1、15,随后500 mg d1每 28天给药。Palbociclib给药方式为 125 mg/d口服给药d1-21、q28d。该项研究的主要终点为PFS,次要研究终点包括总生存、客观反应率以及反应持续时间。这项研究的全部研究结果将会在今年6月的2015 ASCO">ASCO年会上被公布。Palbociclib /氟维司群联合治疗的不良事件发生与先前药物单药使用时的不良反应发生率相似。
根据Ⅱ期PALOMA-1研究结果,palbociclib已进入美国食品与药物管理局(FDA)的加速审批流程,用于一线治疗绝经后ER+、HER2-转移性乳腺癌患者的治疗。在开放的Ⅱ期研究中,来曲唑基础上加用palbociclib联合治疗相比来曲唑单独应用可以显著降低51%的疾病进展风险。联合palbociclib的中位PFS期为20.2个月,单独来曲唑组为10.2个月(HR=0.488,P =.0004)。PALOMA-1试验随机入组165例绝经后ER+、HER2-晚期乳腺癌患者,以1:1比例随机分为两组。来曲唑连续给药2.5 mg qd,palbociclib每日125 mg治疗3周后休息1周,直至疾病进展。主要终点是研究者评估的PFS。3~4级中性粒细胞减少在palbociclib组明显高于来曲唑单药组(54% vs 1%)。此外,3~4级白细胞减少(19% 对0)和疲劳(4%对1%)的发生率palbociclib组均增高。研究中没有发热性中性粒细胞减少或粒细胞减少相关感染的发生。由于副作用导致治疗终止的发生率在palbociclib联合组为13%,在来曲唑单药组为2%。联合治疗组最常见的严重不良事件是肺动脉栓塞(4%)和腹泻(2%)。PALOMA-1共同研究者Dennis Slamon博士表示,“随着FDA的批准,这项研究会改变我们现有的临床实践。palbociclib将成为绝经后妇女ER+/HER2的转移性乳腺癌的标准治疗方法。”
点评
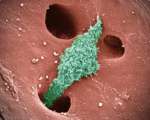
CDK4/6是细胞分裂周期的重要调节蛋白,诱导细胞从G1到S期转化。抑制这两个酶可以阻断细胞的继续分裂,起到肿瘤细胞杀灭作用。临床研究已在淋巴癌、肺癌和乳腺癌患者中观察到临床疗效。随着PALOMA-1结果的公布,CDK4/6抑制剂palbociclib作为一线药物治疗ER阳性、HER2阴性乳腺癌适应症获FDA优先审批权,准备以Ⅱ期临床数据申请上市。验证性Ⅲ期试验PALOMA-2目前正在进行中。PALOMA-2研究比较palbociclib+来曲唑联合对比来曲唑单药用于绝经后ER+、HER2-晚期乳腺癌的一线治疗(NCT01740427)。在PALOMA-2数据公布之前,我们很高兴提前迎来PALOMA-3的结果,为晚期HR+乳腺癌患者,尤其是内分泌治疗后进展患者提供了更多的选择。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












已拜读,受益匪浅。
62
#ASC#
38
看看
183
#palbociclib#
49
#PFS#
41