乳腺X线诊断一直是初级医师诊断的难点,仅书本上的知识难以满足临床需求,如何快速提升乳腺X线诊断水平并应用于临床实践?今天为大家带来《乳腺X线检查系列解读》,希望能给大家起到实质性的帮助。
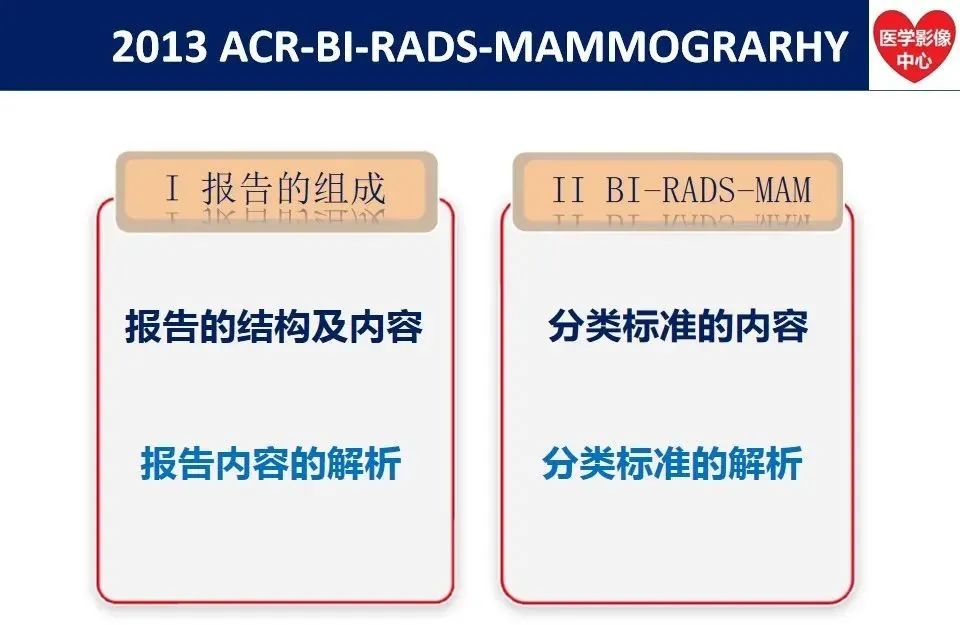
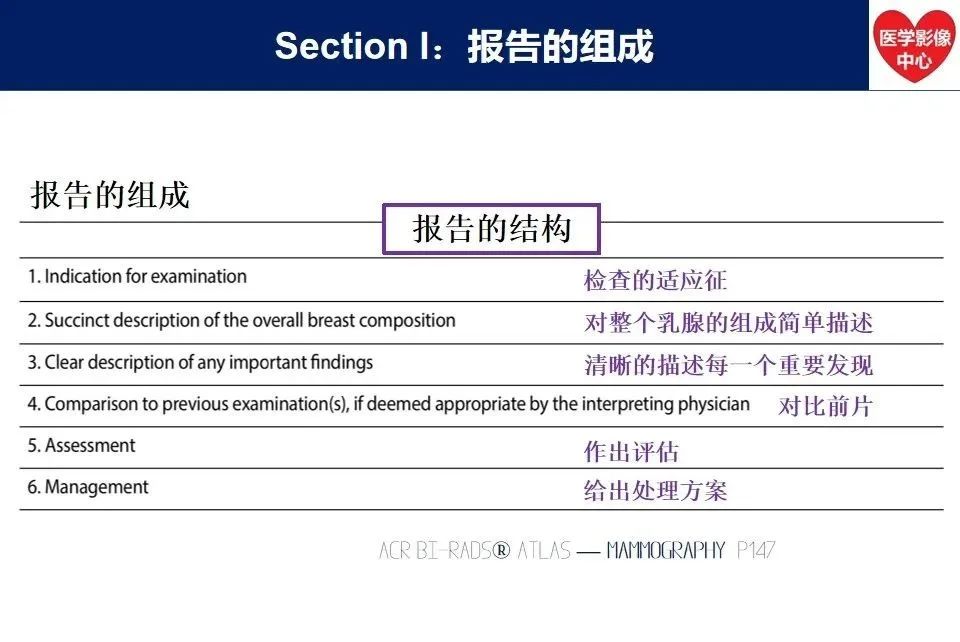
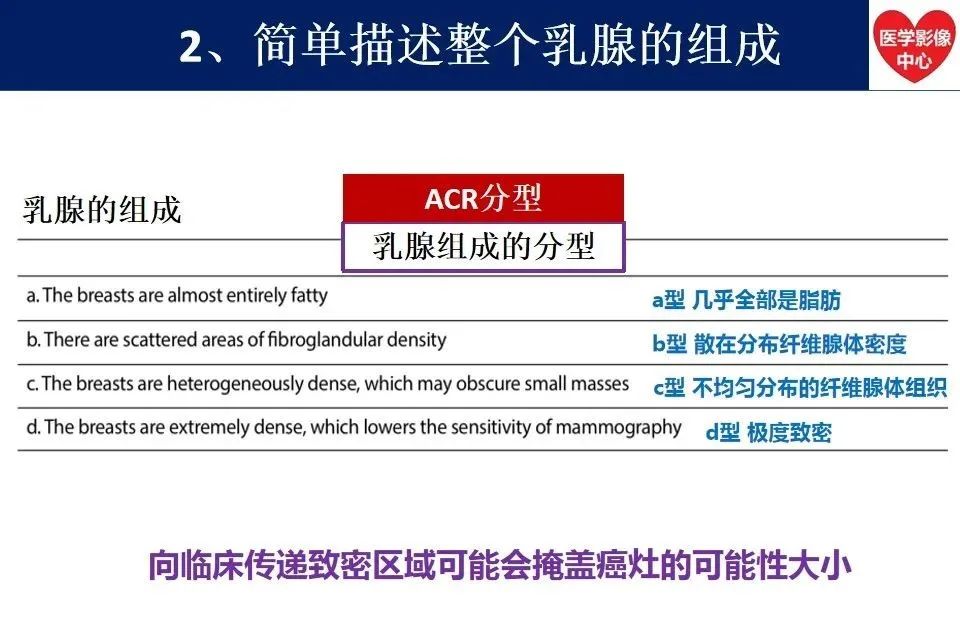
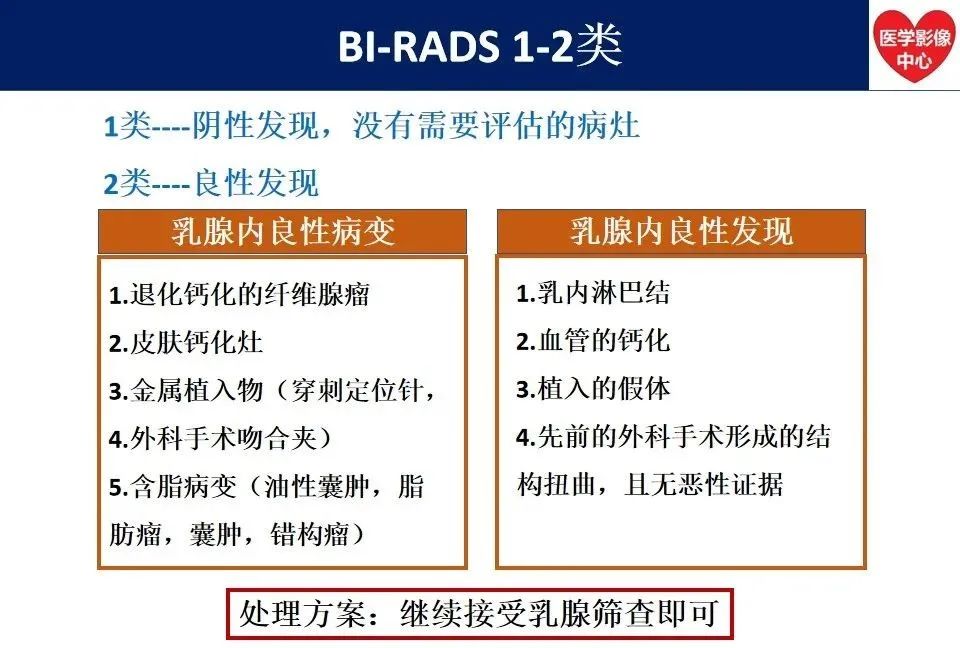
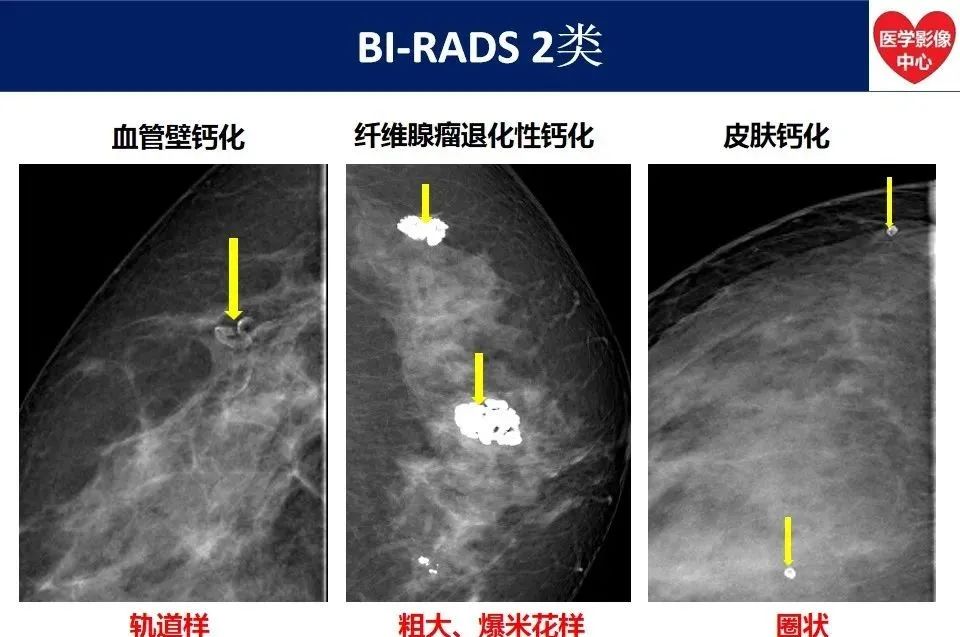
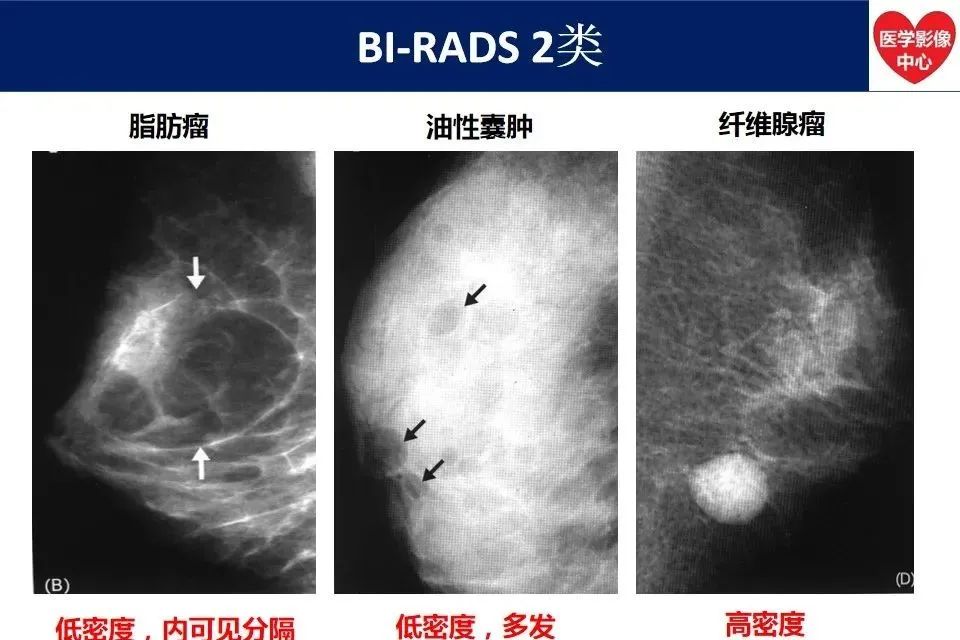
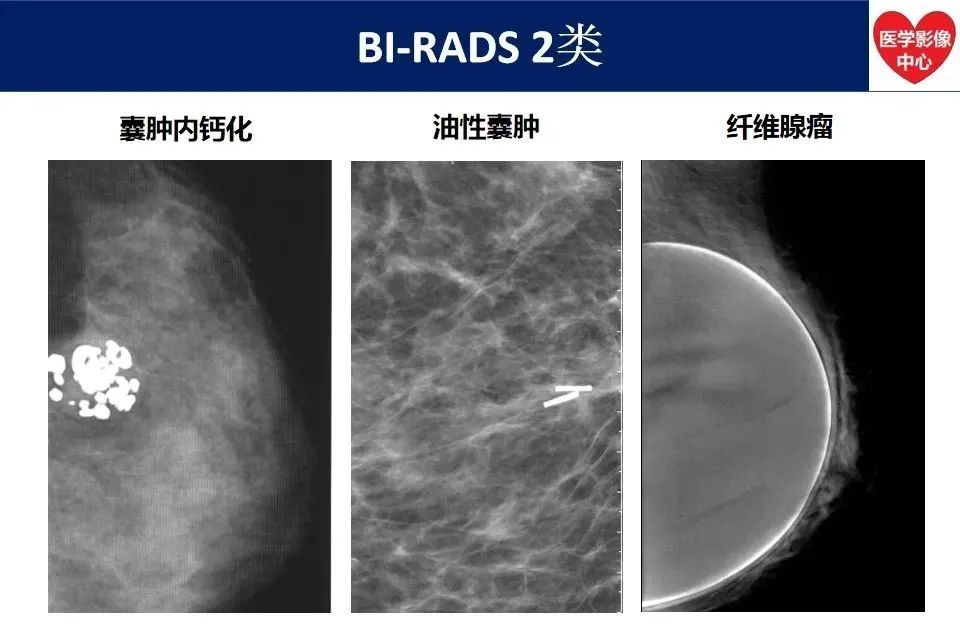
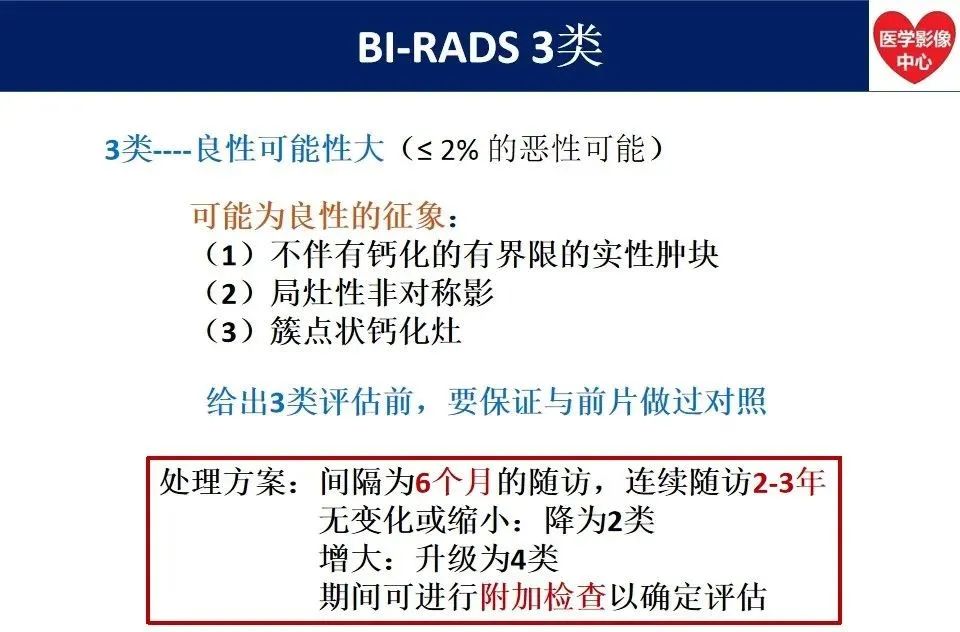
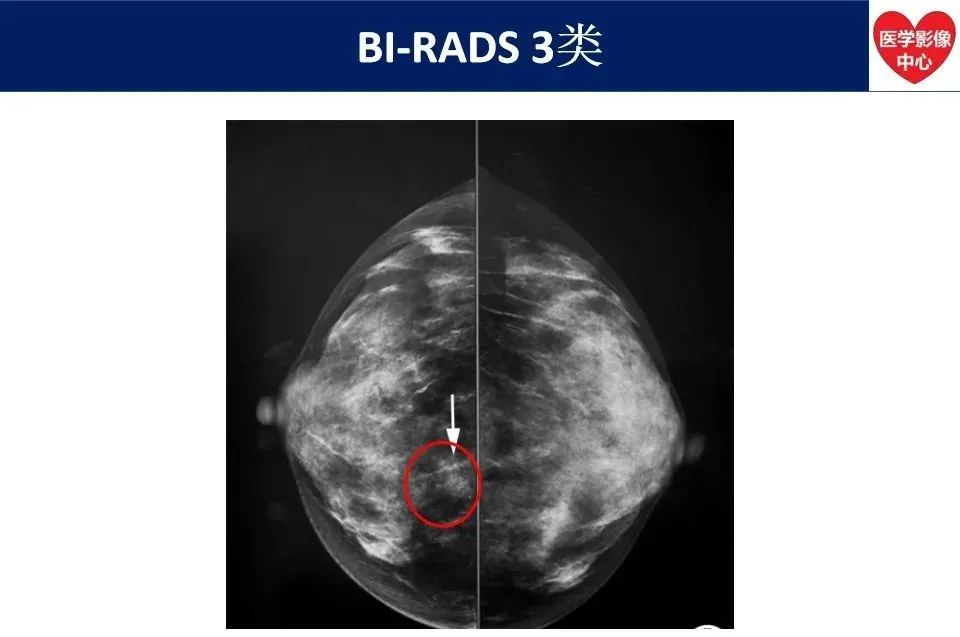
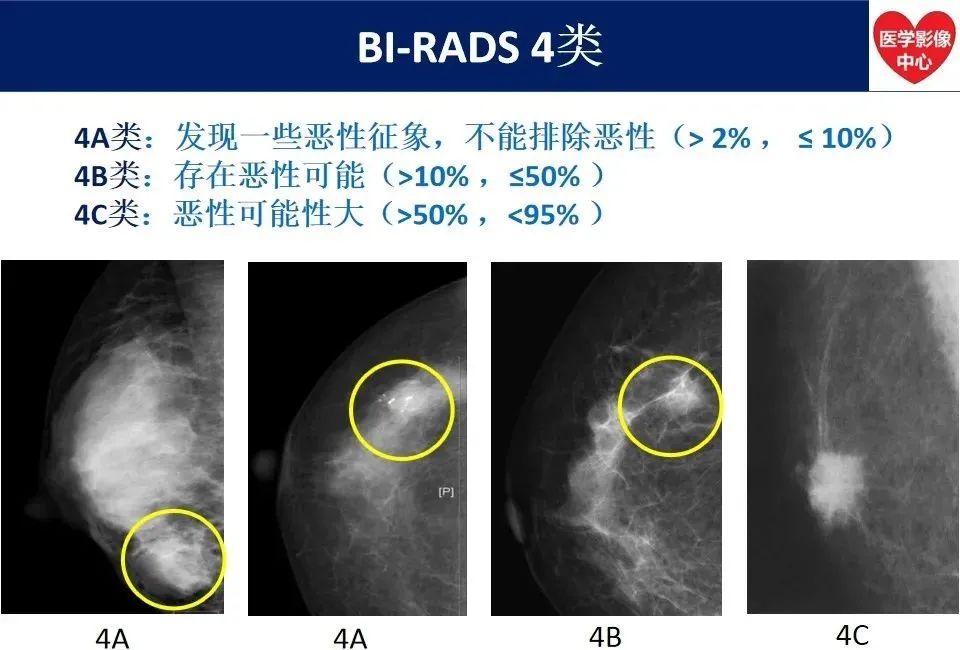
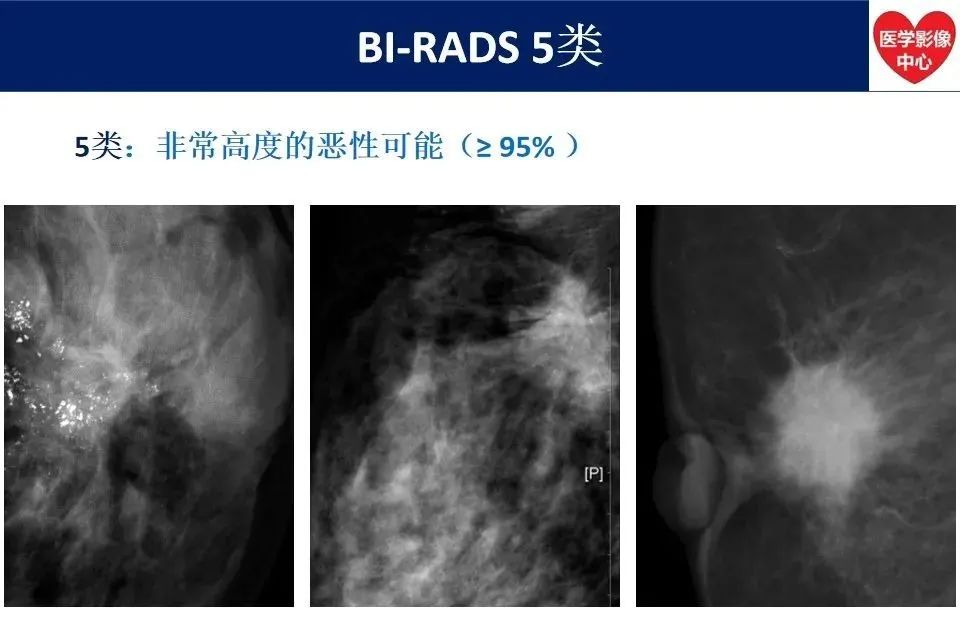
《最新版乳腺X线BI-RADS 分类解读》



本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#ADS#
46
#RADS#
41
#最新#
46
#X线#
0
#BI-RADS#
44