Cell:黑色素瘤劫持重要免疫信号途径对抗免疫治疗
2016-09-28 佚名 生物谷
2016年9月28日讯 /生物谷BIOON/ --来自美国MD安德森癌症中心的研究人员在国际学术期刊Cell上发表了一项最新研究进展,他们发现黑色素瘤能够利用一个重要的免疫应答途径中的基因突变抵抗免疫治疗药物ipilimumab。 IFNγ是一个能够激活免疫应答的细胞因子,除此之外IFNγ还可以通过结合细胞表面的受体直接攻击肿瘤细胞,引发一系列分子事件抑制细胞生长促进肿瘤细胞死亡。研究人员表

来自美国MD安德森癌症中心的研究人员在国际学术期刊Cell上发表了一项最新研究进展,他们发现黑色素瘤能够利用一个重要的免疫应答途径中的基因突变抵抗免疫治疗药物ipilimumab。
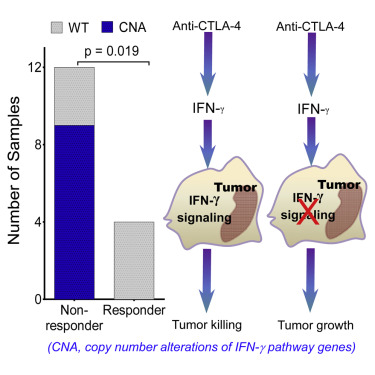
IFNγ是一个能够激活免疫应答的细胞因子,除此之外IFNγ还可以通过结合细胞表面的受体直接攻击肿瘤细胞,引发一系列分子事件抑制细胞生长促进肿瘤细胞死亡。研究人员表示,IFNγ这种直接的细胞杀伤作用可能受到了肿瘤细胞基因突变的阻断。
之前有研究表明ipilimumab治疗会导致Τ细胞合成的IFNγ增加,因此研究人员认为肿瘤细胞在IFNγ信号途径上出现缺陷可能导致抵抗ipilimumab治疗。
他们首先对16名接受ipilimumab治疗的黑色素瘤病人进行了全外显子测序数据分析。16名病人中只有4人应答ipilimumab治疗,另外12人不应答。在不应答治疗者的肿瘤中共发现184个基因突变,其中142个为基因拷贝数变异,42个为单核苷酸变异,而在应答治疗者的肿瘤中只发现了4个基因突变。分析表明不应答治疗者在肿瘤的IFNγ信号途径上平均存在15.33个基因突变,基因拷贝数的变异最为显著。
12个不应答治疗者中有9人存在基因拷贝数的改变,其中一些基因的变异最为显著,包括IFNγ的两个受体IFNGR1和IFNGR2以及两个最重要的下游基因IRF-1和JAK2出现基因缺失。这条通路上两个已知的抑制因子SOCS1和PIAS4出现了基因扩增的情况。
对The Cancer Genome Atlas数据库中367名黑色素瘤病人的生存数据进行分析表明存在基因拷贝数变异的病人生存时间更短,相比于不存在突变的病人短了大约8个月。
研究人员在一个对IFNγ攻击比较敏感的黑色素瘤细胞系中敲除IFNGR1,结果发现肿瘤细胞在存在IFNγ的情况下也可以生长。他们又将相同的细胞系移植到小鼠体内,并用ipilimumab进行治疗,24只存在正常IFNγ受体的小鼠中只有4只发展为癌症,而移植了敲除IFNGR1的细胞系的25只小鼠中有12只发展为肿瘤。
所有未接受治疗的小鼠都死于肿瘤生长,80%接受了ipilimumab治疗并存在正常受体的小鼠存活下来,接受了治疗但受体表达被抑制的小鼠只有一半存活下来。
研究人员表示他们希望找到联合治疗策略克服IFNγ信号途径中一些关键的缺失,“我们希望能够刺激免疫系统产生其他细胞因子,治疗IFNγ信号途径发生损伤的肿瘤。”文章通讯作者Padmanee Sharma这样表示。
原始出处:
Gao J, Shi LZ, Zhao H, Chen J, Xiong L, He Q, Chen T, Roszik J, Bernatchez C, Woodman SE, Chen PL, Hwu P, Allison JP, Futreal A, Wargo JA, Sharma P.Loss of IFN-γ Pathway Genes in Tumor Cells as a Mechanism of Resistance to Anti-CTLA-4Therapy.Cell. 2016 Sep 9. pii: S0092-8674(16)31167-9. doi: 10.1016/j.cell.2016.08.069. [Epub ahead of print]
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#色素#
0
#CEL#
31
#Cell#
33
#信号途径#
28
#黑色素#
24
#黑色素#
18