Pediatr Dermatol:无葡萄膜炎的家族性Blau综合征报告
2018-03-24 cuiguizhong MedSci原创
墨西哥社会医学遗传学研究所医学遗传学中心的Toral-LópezJ近日在Pediatr Dermatol发表了一项工作,他们发现了具有Blau综合征的墨西哥家族,并发现英夫利昔单抗治疗具有良好的治疗效果。
墨西哥社会医学遗传学研究所医学遗传学中心的Toral-LópezJ近日在Pediatr Dermatol发表了一项工作,他们发现了具有Blau综合征的墨西哥家族,并发现英夫利昔单抗治疗具有良好的治疗效果。
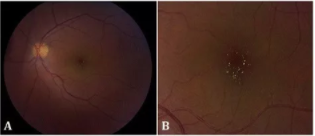
这项研究中的源发病患是一名患有Blau综合征的4岁墨西哥女孩。她和她受感染的家人患有皮疹和关节炎,但没有葡萄膜炎。他们进行外显子组测序,并对来自血液样品的DNA直接测序,发现受影响的家族成员中含有新的核苷酸结合寡聚化结构域的蛋白2基因突变。

这项研究是第一个具有Blau综合征的墨西哥家族的病例报告,研究发现,他们对英夫利昔单抗治疗具有良好的治疗效果。含有核苷酸结合寡聚化结构域的蛋白质2基因(c.1808A> G)中的新突变使得Blau综合征中的突变谱变得更加丰富。
因此,他们认为,这个家族代表了少数几种没有葡萄膜炎的常染色体Blau综合征。由于表型多变,因此确定临床识别Blau综合征的特征和相关的遗传咨询是很重要的。
原文出处:
Toral-Lopez, J., et al., Familial Blau syndrome without uveitis caused by a novel mutation in the nucleotide-binding oligomerization domain-containing protein 2 gene with good response to infliximab. Pediatr Dermatol, 2018.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
33
#DIA#
37
#综合征#
42
#家族性#
40
好
71
谢谢分享学习
57