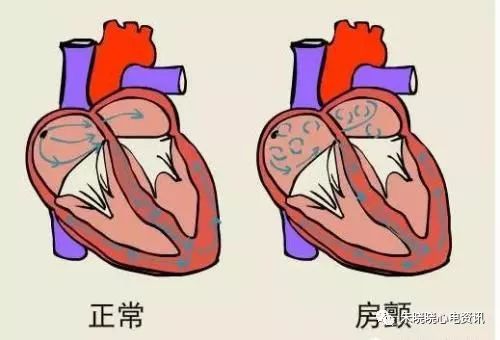
一、心房颤动
房颤典型心电图表现:正常P波消失,代以大小不等、形状各异的颤动波(f波);通常以V1导联最明显;心房颤动波可较粗大,亦可较细小;房颤波的频率为350~600次/分;R-R间距绝对不齐,QRS波一般不增宽。

1.心房颤动心电图诊断注意要点
(1)房颤伴长R-R间期如何报告?心电图危急值:常规心电图≥3.0秒;动态心电图≥5.0秒或出现3次以上≥3.0秒的长R-R间期。出现危急值应及时报告临床医生。
(2)房颤伴室内差异传导与室性早搏的鉴别。
(3)房颤合并三度房室传导阻滞(心电图危急值)。
(4)房颤合并预激综合征与室速的鉴别。
2.房颤伴室内差异传导与室性早搏的鉴别
(1)房颤伴室内差异传导的主要心电图表现:①多发生在心室率较快的情况下;②多有长-短心动周期现象(阿什曼现象);③宽QRS波形态表现为典型右束支阻滞图形或左束支阻滞图形。
(2)房颤合并室早的主要心电图表现:①宽QRS波形态符合室早(室速)的形态特征(建议使用12导心电图记录或12导动态心电图记录);②常有类代偿间歇。
3.阿什曼现象
(1) 定义:指在长R-R间期后提早出现的室上性激动致QRS波形态改变的现象,属于室内差异性传导。
(2)发生机制:心脏传导系统的不应期有一个规律,即心动周期越长不应期也越长;心动周期越短不应期也越短。阿什曼现象常见于房颤,由于心室率不整齐,在长-短心动周期时,常易出现宽大畸形的QRS波群,通常呈现右束支阻滞图形,亦可表现为左束支阻滞图形。
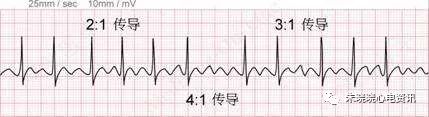
二、心房扑动
房扑典型心电图表现:正常P波消失,代之连续的锯齿状扑动波(F波),F波间无等电位线,波幅大小一致,间隔规则,频率为240~350次/分;F波多数在Ⅱ、Ⅲ、aVF导联上清晰可见,大多不能全部下传,常以固定房室比例(2:1或4:1)下传。如果房室传导比例不恒定或伴有文氏传导现 象,则心室律可以不规则。
1.经典的心房扑动分类
(1)I型房扑(典型房扑):
①常见型:心电图Ⅱ、Ⅲ、aVF导联F波倒置,V1导联F波常为直立;
②少见型:心电图Ⅱ、Ⅲ、aVF导联F波直立,V1导联F波可以直立,也可以倒置。
(2)Ⅱ型房扑(非典型房扑,不纯性房扑):
扑动波的大小和间距不规则,频率340~430次/分,可自行转化为房颤或典型房扑。
2.心房扑动心电图诊断注意要点
(1)频率为300次/分且R-R整齐的心动过速要注意排除房扑1:1传导的可能。
(2)频率为150次/分且R-R整齐的宽QRS波心动过速要注意排除房扑2:1传导的可能(房扑伴室内差性传导,或原有束支阻滞,或合并预激综合征)。
3.心房扑动伴宽QRS心动过速的鉴别诊断
(1)药物难以终止的宽QRS心动过速,而心室率为150次/分(极少数心室率为300次/分)要考虑可能为房扑。食管心电图具有重要的诊断价值(心房波2:1传导)。
(2)宽QRS波如呈典型束支阻滞图形,一般为房扑经房室结下传伴室内差异性传导,如呈类似室速的图形应考虑房扑经预激旁路下传可能。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











赞赞赞
61
#心房颤动#
104
学习
66
#诊断要点#
42
#心房#
38
评论
60