Hypertension:收缩压和长期连续监测房颤筛查对卒中的影响
2022-07-10 MedSci原创 MedSci原创
ILR筛查房颤对血栓栓塞事件的益处随着血压的升高而增加。收缩压≥150mm Hg与≥24小时的房颤发作风险增加>1.5倍相关,同时通过ILR筛查将卒中或全身动脉栓塞的风险降低了近50%。
房颤可使卒中风险增加5倍,通过指南指导的口服抗凝治疗可有效降低卒中风险。植入心血管电子设备的患者大多数房颤发作是无症状的,即使是短暂的房颤发作也与卒中风险增加有关,其中高血压是众所周知的房颤危险因素,但缺乏关于收缩压与连续房颤筛查效果之间相互作用的数据。

近日,心血管权威杂志Hypertension上发表了一篇研究文章,LOOP研究将年龄在70至90岁且具有额外卒中风险因素的未患房颤个体随机分配至使用植入式循环记录器(ILR)进行筛查并在检测到房颤发作≥6分钟后开始抗凝治疗或常规治疗。

该研究总共有5997名具有基线收缩压测量值的参与者被纳入该子研究。研究人员使用特定原因Cox模型中的首次事件发生时间原则分析结局。
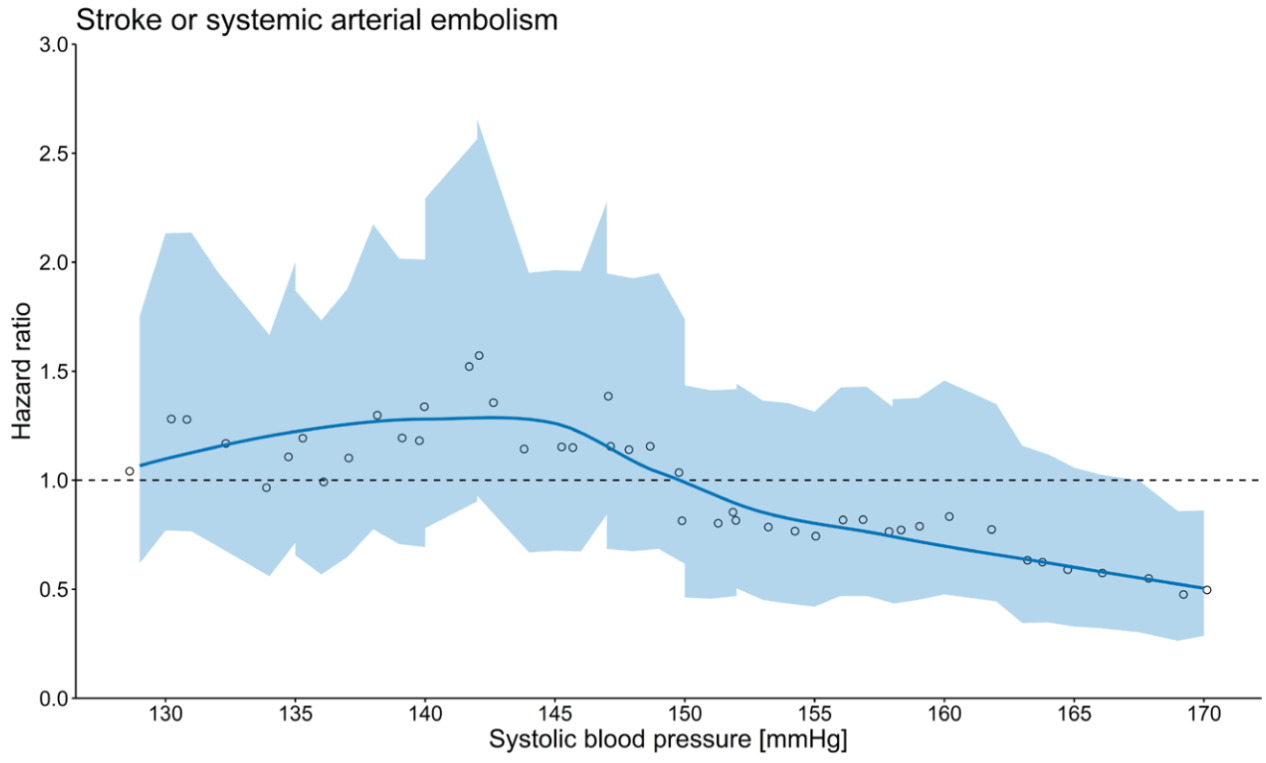
与对照组相比,ILR筛查的卒中或全身动脉栓塞的风险比随着收缩压的增加而降低。在收缩压≥150mmHg的参与者中,ILR筛查使卒中或全身动脉栓塞的风险降低了44%(调整后的风险比为0.56[0.37-0.83])。在ILR组中,收缩压≥150mmHg与24小时以上的房颤事件发生率高于收缩压较低的发生率相关(调整后的风险比为1.70[1.08-2.69]),但与房颤的总体发生率无关(调整后的P>0.05)。
由此可见,ILR筛查房颤对血栓栓塞事件的益处随着血压的升高而增加。收缩压≥150mm Hg与≥24小时的房颤发作风险增加>1.5倍相关,同时通过ILR筛查将卒中或全身动脉栓塞的风险降低了近50%。但是,这些结果应值得进一步研究。
原始出处:
Lucas Yixi Xing.et al.Systolic Blood Pressure and Effects of Screening for Atrial Fibrillation With Long-Term Continuous Monitoring (a LOOP Substudy).Hypertension.2022.https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.122.19333
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#收缩压#
47
#PE#
30
#TENS#
51
#Hypertension#
38
#房颤筛查#
42