Hippocampus: 唤醒老年痴呆症小鼠“失去的”记忆
2017-08-05 佚名 中国生物技术网
“失去的”记忆被恢复了?最近发表在《hippocampus》的一项研究显示,阿尔兹海默症小鼠遗忘的记忆被重新唤醒了。这表明疾病并没有破坏记忆,而是削弱了我们回忆它们的能力。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言





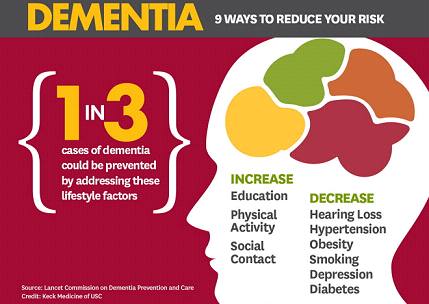







#痴呆症#
27
#CAM#
44
#OCA#
31
#cAMP#
40
老年痴呆症的治疗。
59
学习了
68
学习了
51
学习了
0
认真学习,不断进步,把经验分享给同好。点赞了!
60
唤醒丢失的记忆~
0