STTT:治愈乙肝新希望:新型纳米载体,递送siRNA特异性靶向肝细胞
2022-02-23 王聪 “生物世界”公众号
慢性乙肝的最终目标是临床治愈(功能性治愈),即停止治疗后仍保持HBsAg(乙肝表面抗原)阴性、乙肝病毒DNA检测不到、肝脏生物化学指标正常、肝脏组织病变改善。
由乙型肝炎病毒(HBV)感染引起的乙型肝炎是全球公共卫生的重要威胁。全世界目前有超过3亿人感染乙肝病毒,每年有约60万人死于乙肝病毒导致的肝脏疾病或肝癌。而我国是世界受乙肝疾病负担最重的国家,慢性乙肝患者多达2800万人,其中绝大多数并未接受治疗。
目前针对慢性乙肝的治疗方法包括核苷类似物和干扰素等,但这些都很难实现功能性治愈,因此,亟待开发新的有效疗法。彻底根治慢性乙肝的药物开发面临的主要挑战在于如何消除cccDNA(乙肝病毒整合进入人体基因组后形成的共价闭合环状DNA的稳定形式)、靶向病毒基因组以及克服免疫障碍。
慢性乙肝的最终目标是临床治愈(功能性治愈),即停止治疗后仍保持HBsAg(乙肝表面抗原)阴性、乙肝病毒DNA检测不到、肝脏生物化学指标正常、肝脏组织病变改善。
乙肝药物开发主要以HBsAg(乙肝表面抗原)的持续清除作为衡量功能性治愈的主要参考指标,降低HBsAg是目前临床治疗的主要挑战,也是现阶段乙肝治疗中的最大痛点。因此,寻求一种有效降低HBsAg、安全性好、能达到功能性治愈的抗乙肝病毒药物迫在眉睫。
近日,瑞博生物在 Signal Transduction and Targeted Therapy 期刊发表了题为:Ionizable liposomal siRNA therapeutics enables potent and persistent treatment of Hepatitis B 的研究论文。
该研究开发了一种新型可电离脂质纳米颗粒——RBP131,通过靶向载脂蛋白B(APOB)而特异性进入肝脏细胞,并用其递送靶向乙肝病毒基因组的修饰的siRNA。
动物试验结果显示,RBP131递送的siRNA,能够有效抑制循环系统和肝组织中的乙肝病毒RNA和抗原(HBsAg、HBeAg)以及乙肝病毒DNA。这为慢性乙肝的功能性治愈提供了有前景的治疗方法。
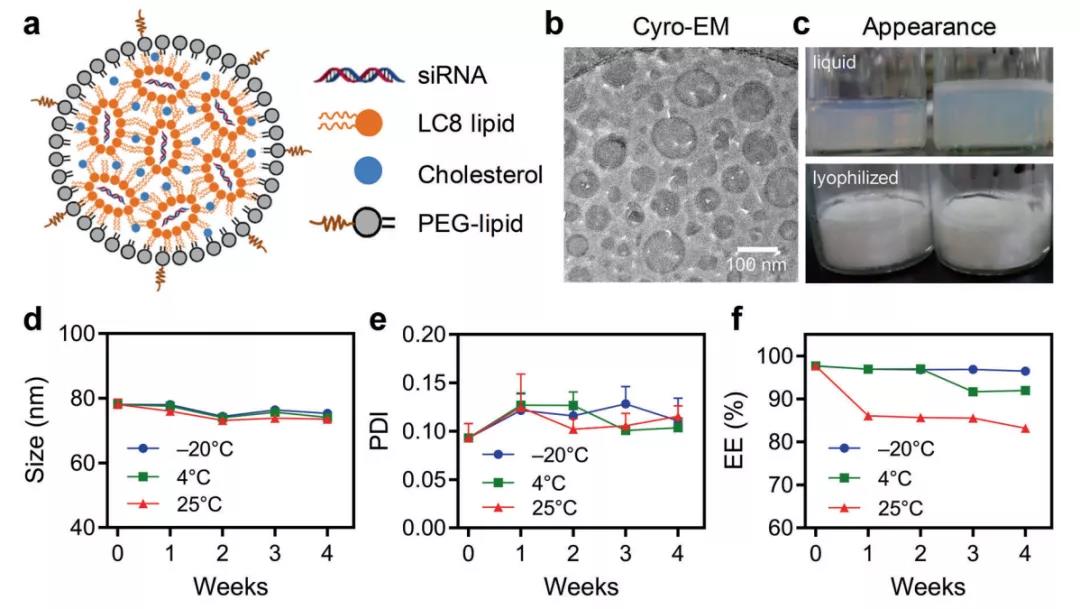
RBP131由瑞博生物专利开发的可电离脂质LC8与脂质PEG和胆固醇配制而成,与siRNA混合后,自组装成具有双层或多层结构的纳米尺度球形囊泡。将其制备成冻干制剂后,在-20°C、4°C或25°C下储存,长达4周时间内,纳米颗粒外观、封装效率、颗粒尺寸、多分散指数和zeta电位保持稳定。
小鼠模型研究显示,在循环系统和肝组织中,乙肝病毒RNA和抗原(HBsAg、HBeAg)以及乙肝病毒DNA的表达并显着抑制,且呈剂量依赖性和时间依赖性。相比之下,现在临床一线用药核苷类似物药物恩替卡韦几乎没有抑制抗原表达。
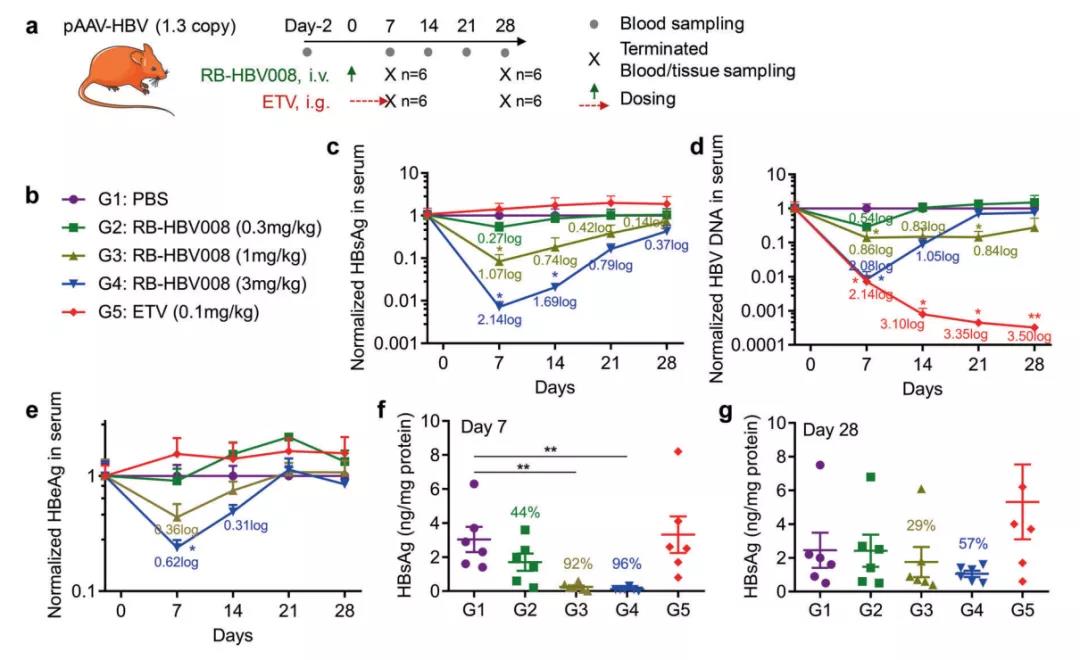
这项研究表明,脂质纳米颗粒RBP131递送siRNA有望长效持久治疗乙肝。
总的来说,该研究开发了一种基于LC8的新型可电离脂质纳米颗粒递送载体,能够特异性靶向肝细胞,用来向干细胞递送siRNA,在小鼠和大鼠模型上,展现了功能性治愈慢性乙肝的巨大前景。而且这种纳米颗粒递送载体可制备成冻干粉,稳定性更强,便于保存和运输。
原始出处:
Huang, Y., Zheng, S., Guo, Z. et al. Ionizable liposomal siRNA therapeutics enables potent and persistent treatment of Hepatitis B. Sig Transduct Target Ther 7, 38 (2022). https://doi.org/10.1038/s41392-021-00859-y.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#载体#
49
#肝细胞#
50
#纳米载体#
50
#特异性#
37
#新希望#
47
#siRNA#
60