Invest Ophthalmol Vis Sci:脉络膜肿胀对视神经乳头变形的影响
2018-08-20 cuiguizhong MedSci原创
美国乔治亚理工学院生物医学工程系和VA医疗中心视觉和神经认知康复中心的Feola AJ近日发表文章指出,他们开发了一个有限元模型,用来研究急性脉络膜肿胀如何影响视神经乳头(ONH)变形。
美国乔治亚理工学院生物医学工程系和VA医疗中心视觉和神经认知康复中心的Feola AJ近日发表文章指出,他们开发了一个有限元模型,用来研究急性脉络膜肿胀如何影响视神经乳头(ONH)变形。
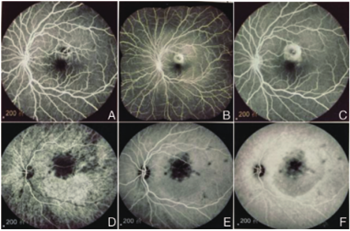
目前已经有研究指出,脉络膜几何形状和肿胀有助于眼病变的发展。因此,了解脉络膜如何影响视神经乳头(ONH)生物力学环境是很重要的。他们开发了ONH的两个几何模型:一个具有"钝的"脉络膜插入模型,另一个具有"锥形"脉络膜插入模型。他们检查了脉络膜体积变化-估计在眼脉冲期间发生约2.1-14.2μL,以及体积变化如何影响早期神经组织、筛板和逆向神经组织等三个组织区域的生物力学变化。然后,他们进行了灵敏度分析,以了解ONH压力、组织材料特性和脉络膜肿胀的变化如何影响峰值组织应变情况。
经过分析,结果发现,钝性脉络膜几何形状中的脉络膜肿胀对前层神经组织中的应变具有很大的影响,其大小与30mm Hg的IOP发生的大小相当。锥形脉络几何形状中的脉络膜肿胀也有影响,但与钝性几何形状相比程度较小。灵敏度分析证实,脉络膜肿胀对钝性脉络膜几何形状的早期神经组织应变影响更大。
因此,他们认为,脉络膜解剖结构和肿胀可以相互作用,在早期神经组织变形中起重要作用。这些研究结果表明,脉络膜可能在ONH生物力学中起着重要的,这是在之前没有被认可的作用。同时,他们认为需要进一步研究以更好地了解脉络膜体积变化在生物体内的效应。
原文出处:
Feola, A.J., et al., The Impact of Choroidal Swelling on Optic Nerve Head Deformation. Invest Ophthalmol Vis Sci, 2018. 59(10): p. 4172-4181.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#视神经#
32
#EST#
28
#视神经乳头#
43
#脉络膜#
27
#脉络膜肿胀#
30
#THA#
33