Int J Cardiol:白细胞介素-1受体拮抗剂对冠心病患者预后的影响!
2018-02-02 xing.T MedSci原创
由此可见,IL 1-Ra是CAD患者不良结局的独立的预测指标,尤其在ACS情况下,其超过了hs-CRP和肌钙蛋白T的预后价值。对于CAD患者,该研究发现可能会改善次级预防的风险评估和抗炎治疗的患者选择。
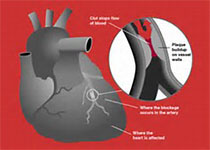
IL-1β介导的炎症反应会促进冠心病(CAD)的发生和发展。近日,心血管领域权威杂志International Journal of Cardiology上发表了一篇研究文章,研究人员旨在评估炎症标志物白细胞介素-1受体拮抗剂(IL1-Ra),反映IL-1β活性,对CAD患者预后的影响。
研究人员测量了AtheroGene研究中1337名受试者的IL-1Ra水平,前瞻性心血管登记中心纳入了通过冠状动脉造影表现为急性冠状动脉综合征(ACS)和稳定型心绞痛的CAD患者。中位随访时间为6.4 年。
IL1-Ra水平处于最高三分位数范围的患者更常表现为ACS(55% vs. 40% vs. 34%,P<0.001),更常见采用PCI治疗(47% vs. 39% vs. 34%,P<0.001),并且有较低的左室射血分数(LVEF)(61±15% vs. 62±15% vs. 65±14%,P=0.001)和较高 hs-CRP水平(10 vs. 4.2 vs. 2.5mg/L,P<0.001)。对传统的心血管危险因素、LVEF、hs-CRP和肌钙蛋白T进行调整后,IL1-Ra基线水平对总体研究人群全因死亡率具有预测作用(调整后的风险比为1.45(95%可信区间为1.16-1.82),P<0.001)。在ACS患者的亚组中,而不是那些稳定型心绞痛患者中,IL1-Ra是心血管死亡的独立预测因子(ACS:调整后的风险比为1.85(95%可信区间为1.33-2.58),P<0.001;稳定型心绞痛:调整后的风险比为1.25(95%可信区间为0.95-1.65),P=0.11)。
由此可见,IL 1-Ra是CAD患者不良结局的独立的预测指标,尤其在ACS情况下,其超过了hs-CRP和肌钙蛋白T的预后价值。对于CAD患者,该研究发现可能会改善次级预防的风险评估和抗炎治疗的患者选择。
原始出处:
Niklas Schofer,et al. Prognostic impact of Interleukin-1 receptor antagonist in patients with documented coronary artery disease.International Journal of Cardiology.2018. https://doi.org/10.1016/j.ijcard.2018.01.055
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#Cardiol#
27
#患者预后#
24
#冠心病患者#
32
#拮抗剂#
0
#白细胞介素#
33
学习一下谢谢
35