本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
2018-01-23 李京艳 医学界内分泌频道
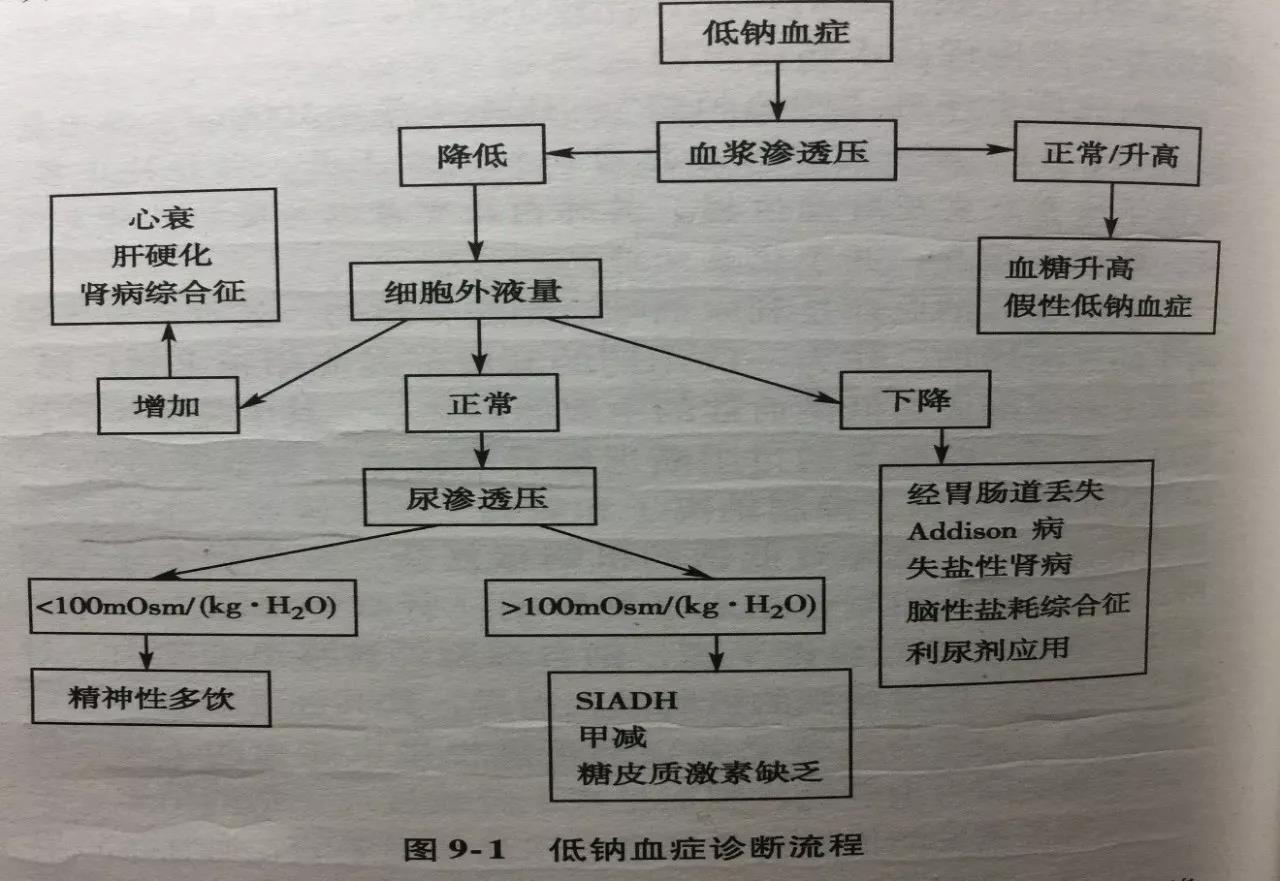
老人家因心律失常和高血压入院,却在住院期间意外出现低钠血症,谁是元凶?

英国学者的一项研究表明,替换药物或添加阿米洛利可能是预防噻嗪类诱导糖尿病的解决方案。论文于2012年4月9日在线发表于《高血压》(Hypertension)杂志。 高血压指南建议限制噻嗪类利尿剂用量并避免联用β受体阻滞剂,原因在于其可升高糖尿病风险。研究者实施了两项双盲、安慰剂对照、交叉研究。在纳入41例患者的第一项研究中,苄氟噻嗪治疗4周后可检查到2小时口服糖耐量试验时的血糖
1.碳酸酐酶抑制剂 代表药物— 乙酰唑胺 • 碳酸酐酶主要存在于肾皮质、红细胞、中枢神经系统、胃黏膜、眼睫状上皮细胞 • 利尿作用弱、易产生耐受性 • 长期应用可引起“代酸”,可治疗“代碱” • 可减少房水形成降眼压,缓解青光眼症状 • 可抑制脑组织及脉络
英国学者的一项研究表明,替换药物或添加阿米洛利可能是预防噻嗪类诱导糖尿病的解决方案。论文于2012年4月9日在线发表于《高血压》(Hypertension)杂志。 高血压指南建议限制噻嗪类利尿剂用量并避免联用β受体阻滞剂,原因在于其可升高糖尿病风险。研究者实施了两项双盲、安慰剂对照、交叉研究。在纳入41例患者的第一项研究中,苄氟噻嗪治疗4周后可检查到2小时口服糖耐量试验时的血糖
噻嗪类利尿剂具有肯定的降压效果、可靠的靶器官保护作用以及良好的安全性和耐受性,但是目前临床中应用很少。2009年China STATUS研究分析了92家三甲医院5086例高血压患者,发现我国高血压人群利尿剂使用率仅10%。利尿剂是各国高血压指南中毫无争议的一线降压药物。然而,由于很多临床医生对此来药物的安全性存在不正确的认识,导致其临床作用与优势未能充分发挥。
英国学者的一项荟萃分析表明,氢氯噻嗪、氯噻酮和苄氟噻嗪在效力方面存在显著差异,这可能解释了标准剂量氢氯噻嗪和氯噻酮的降压效果差异。论文于2012年4月30日在线发表于《高血压》(Hypertension)杂志。 噻嗪类和噻嗪样利尿剂被广泛用于高血压治疗,但近来对氢氯噻嗪和氯噻酮在降压和心血管疾病预防方面的等效性有所质疑。此项研究对3种广泛应用噻嗪类利尿剂(氢氯噻嗪、氯噻酮和苄氟噻嗪)与血


梅斯医学MedSci APP
医路相伴,成就大医
#噻嗪#
27
#低钠血症#
33
#低钠#
24
学习了受益匪浅
52
学习了.谢谢分享.
66
好
56