NEJM:胸腔镜技术与肺萎缩
2015-05-08 陈说 译 MedSci原创
一名46岁肝病终末期的女士,近来频繁地出现反复性肝性胸水和呼吸困难症状,我们对其行胸腔穿刺术治疗。在胸部检查中,右侧胸部听诊未闻及呼吸音。X线检查结果发现,右侧胸部存在液气胸(图A:箭头所指处为气胸;星号所示为胸腔积液)。我们通过猪尾导管将胸水引流出来,但气胸的问题并未能得到解决(图B所示处)。在计算机断层扫描(CT)中,结果显示右侧肺已萎缩和右侧胸膜脏层增厚,没有发现有支气管梗阻的迹象(如图C所
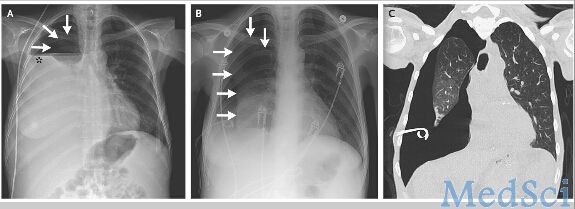
在本案例中,该女士的右侧肺部萎缩是由于脏胸膜纤维发生增厚病变,这是一种慢性炎性过程,继而发展到阻碍了肺部的复张功能,而壁层胸膜没有分离,当脏壁胸膜间隙充满体液的时候,从而形成了液气胸。
医生对病人进行胸腔引流后,由于脏胸膜的纤维增厚导致该患者的肺部仍然无法正常地复张,反而在胸膜腔隙内出现了真空现象。在排除了其他一些可能导致肺部不能完全复张的因素后(如支气管梗阻导致气体无法到达支气管末端充斥肺泡),他们决定采取手术切除脏层胸膜纤维增厚的组织以便恢复底部肺的扩张和功能。
最后,医生通过胸腔镜手术对其肺部胸膜的纤维组织进行剥离清除并将胸膜固定,令人欣慰的是,术后该女士的肺部扩张效果良好,目前已恢复正常的肺功能。
Jeffrey Albores, M.D., and Tisha Wang, M.D.Trapped Lung.N Engl J Med 2015; 372:e25May 7, 2015DOI: 10.1056/NEJMicm1404964
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#肺萎缩#
36
不错的技术!
148
#萎缩#
42
#胸腔镜#
31
看看
122