JACC:优化移植策略可降低生物可吸收血管支架血栓形成的发生率
2016-02-23 崔倩 译 MedSci原创
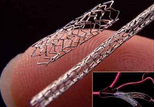
最近的报告表明生物可吸收血管支架(BVS)血栓形成(支架血栓形成[ScT])的发病率升高。这项研究调查在2家德国和2家瑞士的医院中所有接受植入BVS的患者ScT的发生率,临床和血管造影特点,以及可能机制。共有连续的1305例患者(平均年龄64岁,78%为男性)接受1870次BVS(平均1.4±0.8 BVS/例)。研究人员检查了临床/手术特征,死亡率(范围312-652天)和485天时SCT的数据
最近的报告表明生物可吸收血管支架(BVS)的血栓形成(支架血栓形成[ScT])的发病率在升高。
这项研究在2家德国医院和2家瑞士医院中进行的调查,参与者是接受植入BVS的患者,调查ScT的发生率,临床和血管造影特点,以及可能机制。
共有连续的1305例患者(平均年龄64岁,78%为男性)接受1870次BVS(平均1.4±0.8 BVS/例)。研究人员检查了临床/手术特征,死亡率(范围312-652天)和485天时ScT的数据。
共有42例患者发生ScT。可能或明确的ScT的发生率在30天及在12个月分别为3.0%和1.8%,无明显差异(p=0.60)。共有22例(52%)ScTs表现为ST段抬高心肌梗死,6例(17%)为心源性猝死。在多变量分析中,鼻窦病变(P=0.049)和受损左室射血分数(P=0.019)与ScT独立相关。9例ScT(21%)发生在曾暂停双重抗血小板治疗的患者中,6例发生在早产患者中。较低的手术后最小管腔和参照血管直径为ScT的标志(所有P<0.0001)。当手术后最小管腔直径低于2.4mm(为2.5〜3.0mm BVS)和2.8mm(为3.5mm BVS)时,ScT的风险迅速增加。当特定BVS植入策略实施以来,12个月的ScT率从3.3%下降到1.0%,当调整多变量倾向评分后,效果仍然显著(P=0.012;风险比:0.19; 95%置信区间:0.05-0.70)。
ScT的12个月发生率达到3%;在采用一个优化的移植策略后,ScT发生率可能会显著减少。
原始出处:
Serban Puricel,Florim Cuculi,Melissa Weissner,et al.Bioresorbable Coronary Scaffold Thrombosis,JACC,2016.2.23
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#JACC#
29
#可吸收#
25
#生物可吸收#
26
#发生率#
20
#ACC#
20
#支架血栓#
35