Movement disorders:神经影像新发现:帕金森患者,胆碱能神经支配发生改变
2022-02-19 Freeman MedSci原创
胆碱能神经支配的改变已经存在于新生的PD患者中。
认知障碍在帕金森病(PD)中很常见,是导致残疾和生活质量下降的主要原因。25%至30%的新诊断患者已经存在轻度认知障碍(PD-MCI),是PD痴呆(PDD)发展的主要风险因素。
 PD的认知障碍是异质性的,有多个领域受到影响,在发病和进展方面有很大的差异性。人们越来越认识到,合并的胆碱能功能障碍是PD认知障碍的病理生理学的一个主要因素。
PD的认知障碍是异质性的,有多个领域受到影响,在发病和进展方面有很大的差异性。人们越来越认识到,合并的胆碱能功能障碍是PD认知障碍的病理生理学的一个主要因素。
人类大脑的四个主要胆碱能系统是基底前脑(BF)皮质瓣投射系统、小脑幕-外侧被膜复合体(PPN/LDTC)的胆碱能流出物、内侧前庭核(MVN)投射到小脑的胆碱能神经元,以及纹状体胆碱能间神经元。
以前使用乙酰胆碱酯酶正电子发射断层扫描(PET)对胆碱能神经支配的体内神经影像学评估表明,PD主要是后部胆碱能神经支配,PDD的胆碱能变性更严重。还有证据表明,即使在没有痴呆的情况下,胆碱能系统也是PD认知障碍的主要驱动因素。我们以前表明,注意力、执行功能和记忆力的缺陷与全脑皮质水平和区域(亚)皮质水平上的胆碱能活动的丧失相关。
尽管在认知障碍的PD患者中已显示出胆碱能神经支配,但对疾病早期和认知变化发生前的胆碱能神经支配变化了解甚少。在疾病的早期阶段阐明认知障碍和胆碱能完整性之间的关系可能会提供新的线索,为新的治疗策略提供参考。
藉此,荷兰格罗宁根大学的Sygrid van der Zee, PhD等人,描述新诊断的、有或没有认知障碍的治疗,未用药的PD患者的胆碱能神经支配状态。他们比较了新患者(有或没有MCI)和健康对照组(HCs)之间的乙酰胆碱转运体(VAChT)[18F]fluoroethoxybenzovesamicol -([18F] FEOBV)PET成像。
他们纳入了57名新诊断的、未经治疗的PD患者(32名男性,平均年龄64.6±8.2岁)和10名健康对照组(5名男性,平均年龄54.6±6.0岁)。所有参与者都接受了胆碱能[18 F]fluoroethoxybenzovesamicol-PET和详细的神经心理学评估。PD患者被分类为认知正常(PD-NC)或轻度认知障碍(PD-MCI)。进行了基于全脑体素的分组比较。
结果显示,PD的胆碱能神经支配有双向变化。
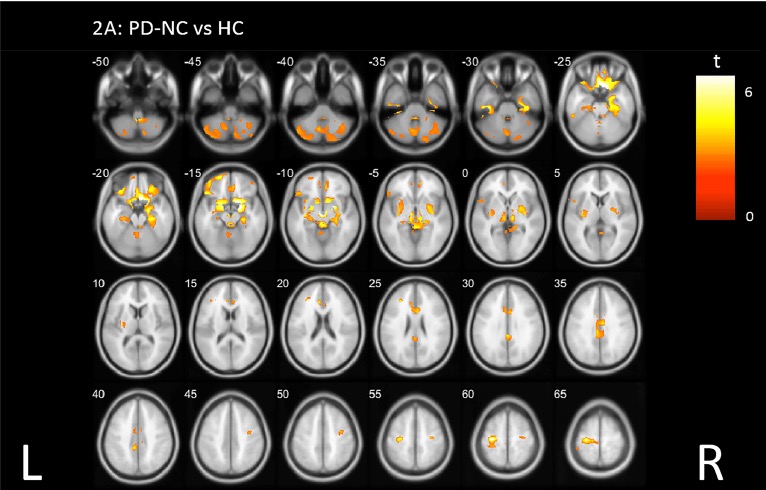
与对照组相比,PD-NC组和PD-MCI组都表现出明显的皮质胆碱能神经支配(P<0.05),主要是在后部皮质区域。
在PD-NC中,高于正常水平的结合在皮质和皮质下区域最为突出,包括小脑、扣带皮层、普陀门、直回、海马和杏仁核。
该研究的重要意义在于发现了:胆碱能神经支配的改变已经存在于新生的PD患者中。所有患者的后皮质胆碱能损失与认知状态无关。在认知完整的患者中,小脑、额叶和皮层下区域的结合力高于正常水平,这可能反映了早期PD的胆碱能补偿性上调。有限的或失败的胆碱能上调可能在PD早期、临床明显的认知障碍中发挥重要作用。
原文出处:
[Zee S, Kanel P, Gerritsen MJJ, et al. Altered Cholinergic Innervation in De Novo Parkinson’s Disease with and without Cognitive Impairment. Movement Disorders. Published online January 17, 2022:mds.28913. doi:10.1002/mds.28913](https://doi.org/10.1002/mds.28913)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#disorders#
39
#ERS#
36
#Dis#
44
#Disord#
37
#新发现#
51
#disorder#
45
#神经影像#
47
#胆碱#
51