NEJM: 甲硝唑过量应用致中毒性脑病-案例报道
2016-04-15 MedSci MedSci原创
http://www.nejm.org/doi/full/10.1056/NEJMicm1505174?query=featured_clinical-practice
男性,58岁,以往患有隐源性肝硬化病史,近日因在家中意外摔倒导致意识不清而被送往ICU收治。
据了解,该患者之前曾因感染破伤风杆菌而应用过甲硝唑抗生素(500 mg,每日三次,为期3周)进行抗菌治疗。
在其被送往医院的前几天,该患者开始出现构音障碍和步态不稳的症状,当时怀疑是与天气的气候变化有关。
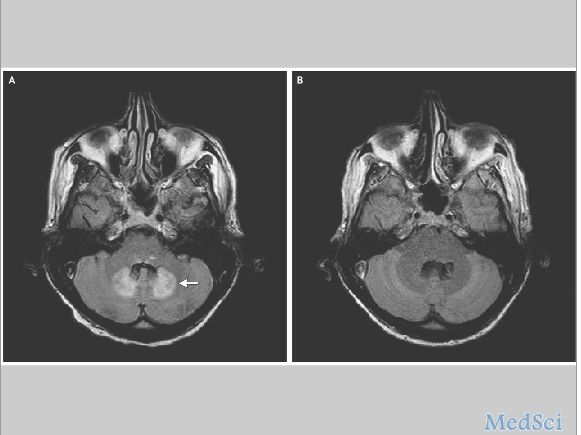
脑部磁共振成像检查结果显示,小脑齿状核部位出现对称性、增强的液体衰减反转恢复信号(如图A,箭头处),该表现与以往中应用甲硝唑抗生素过量导致中毒性脑病是一致的。
入院后,会诊医师即对其进行气管插管辅助通气和镇静治疗。不久,取中心静脉导管做尖端培养发现中心静脉导管相关性菌血症。
随机,会诊医师对其停止甲硝唑药物使用,1个月后作影像学检查的结果如图B所示。
此外,对其进行神经系统方面的评估时,发现该患者神经系统方面的损害已无法恢复。
最后,由于该病人在住院期间发生了中心静脉导管相关性菌血症,而最终死于并发症。
在临床上,甲硝唑过量使用致中毒性脑病是一种非常罕见的药物副作用表现。其典型的症状表现为构音障碍和步态不稳等。而导致中毒性脑病的危险因素与肝功能不全的患者长期应用甲硝唑药物和甲硝唑药物过量使用(累积应用剂量>20g)等有密切的关系。
通常情况下,大脑磁共振成像检查是诊断该病的最常见手段之一,因为在小脑齿状核部会出现对称性增强的信号。
Dimitrios Farmakiotis, M.D.Barry Zeluff, M.D. Metronidazole-Associated Encephalopathy N Engl J Med 2016; 374:1465April 14, 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#脑病#
26
继续学习
60
继续关注
47
好文章值得收藏
49
#甲硝唑#
25
#中毒#
32