Cerebrovasc Dis:卵圆孔未闭介入治疗有效预防隐源性卒中复发
2018-04-18 国际循环编辑部 国际循环
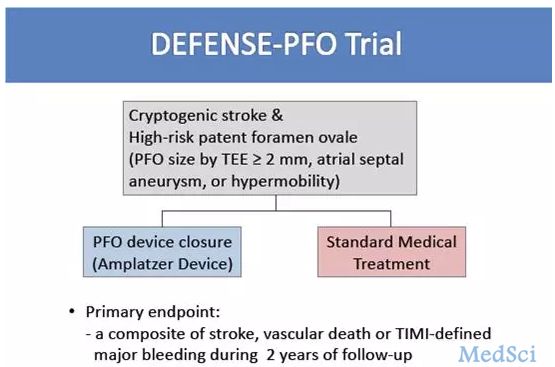
卵圆孔未闭(PFO)合并房间隔膨胀瘤(ASA)患者是隐源性卒中的主要易发群体。经皮穿刺介入治疗PFO与药物治疗两种方法孰优孰劣,学界仍存在巨大分歧,研究者希望通过荟萃分析的方式,找出更为安全有效预防卒中复发的选择。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#隐源性卒中#
0
#ASC#
41
#Dis#
35
#卒中复发#
33
卒中虽然是临床上常见病,溶栓,取栓等血管内治疗也很成熟,但是仍然有很多未知问题有待认知!
56
^_^^_^^_^^_^
72
谢谢分享学习了
63