JAMA Pediatr:十年期间美国婴儿发生围产期艾滋病毒感染现状
2017-03-23 MedSci MedSci原创
目前,可以通过抗逆转录病毒治疗和预防来减少人类免疫缺陷病毒(HIV)在围产期的传播。尚需对围产期艾滋病毒传播和漏失预防机会的数据进行统计,以监测消除母婴传播艾滋病毒的进展情况。近期,一项发表在杂志JAMA Pediatr上的研究旨在评估美国出生的婴儿中发生围产期艾滋病毒病例的数量。此项研究的数据来自国家艾滋病监测系统,统计2002年至2013年(截至2015年12月31日期间),美国(包括哥伦比亚
目前,可以通过抗逆转录病毒治疗和预防来减少人类免疫缺陷病毒(HIV)在围产期的传播。尚需对围产期艾滋病毒传播和漏失预防机会的数据进行统计,以监测消除母婴传播艾滋病毒的进展情况。
近期,一项发表在杂志JAMA Pediatr上的研究旨在评估美国出生的婴儿中发生围产期艾滋病毒病例的数量。
此项研究的数据来自国家艾滋病监测系统,统计2002年至2013年(截至2015年12月31日期间),美国(包括哥伦比亚特区)出生的艾滋病毒婴幼儿和其母亲的数据。根据从出生到诊断和报告时间合并的模式,对每个报告病例进行加权,对诊断和报告的延迟进行了调整。分析于2016年4月1日至8月15日进行。
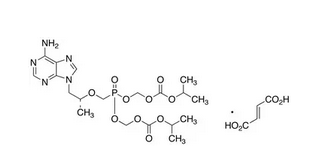
此项研究的暴露因素是孕产妇感染艾滋病毒和使用抗逆转录病毒药物。
此项研究结果显示:在美国出生的围产期感染婴儿估计数从2002年的216(95%CI,206-230)下降到2013年的69(95%CI,60-83)。在2002-2013年出生的围产期艾滋病毒感染儿童中,836名患儿(63.0%)的母亲被确定为黑人或非裔美国人;243名(18.3%)为西班牙裔或拉丁裔。
2002 - 2005年期间,共有236例(37.5%)的母亲在怀孕前诊断出艾滋病毒感染,而2010 - 2013年为120例(51.5%);在2002 - 2005年期间,接受全部3个推荐的抗逆转录病毒预防或治疗药物(产前,产后和出生后)的母婴对的比例为22.4%,而2010-2013年为31.8%,其中约179例(28.4%)(2002- 2005年)和94例(40.3%)(2010-2013年)在怀孕期间接受抗逆转录病毒预防或治疗。
整个研究期间,美国五大南部州(佛罗里达州,德克萨斯州,格鲁吉亚,路易斯安那州和马里兰州)占美国感染艾滋病毒婴儿的687人(38.0%)。根据国家生活活动情况,2013年美国出生的婴儿中,围产期HIV感染发生率为每10万活产婴儿有1.75人。
此项研究表明:尽管美国的围产期艾滋病毒感染减少,但是近年来,受感染婴儿及其母亲的预防机会也经常错失。疾病控制和预防中心拟议的消除母婴传播艾滋病毒的目标是每10万活产婴儿中1人,但截至2013年,围产期艾滋病毒感染的发生率仍然是这一目标的1.75倍。
原始出处:
Taylor AW, Nesheim SR, et al. Estimated Perinatal HIV Infection Among Infants Born in the United States, 2002-2013. JAMA Pediatr. 2017 Mar 20. doi: 10.1001/jamapediatrics.2016.5053.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#DIA#
35
#PE#
37
#艾滋病毒感染#
34
很好
71
非常好的研究
73
签到学习了很多
69