【一般资料】
男,35岁
【现病史】
4个月前不慎咬破左颊黏膜,第2天左面部出现肿痛,行消炎治疗2周后,疼痛消失,包块无明显缓解,生长较快。
【既往史】
右侧后牙反复疼痛史。
【体格检查】
左面颊部明显隆起,大小约7.0cm×6.0cm,触诊质硬,边界清楚。下唇无麻木。开口度约0.5cm。34-44固定义齿修复,48近中阻生,35-37正常。36向后至下颌支牙槽骨颊侧膨隆。伸舌左侧偏斜。双侧腮腺及下颌下腺导管正常。双侧颞下颌关节区无压痛。左侧胸锁乳突肌中上1/3交界处可触及一约0.5cm×0.5cm大小肿大淋巴结,边界清楚,活动度中等,无触压痛。
【辅助检查】
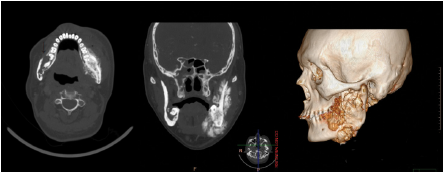
CT显示下颌骨左侧成骨性改变,右下颌角区溶骨性改变(图1)。
【治疗】
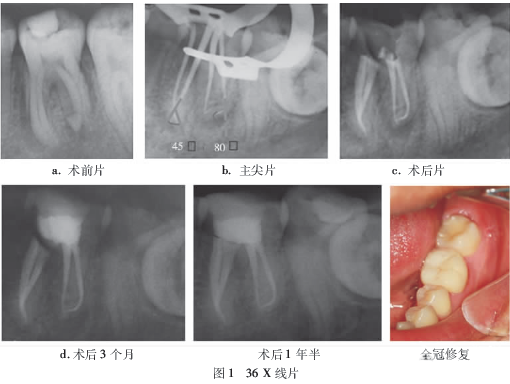
全麻下行下颌骨部分切除术+颌骨骨髓炎刮治术。术中见肿瘤与表面肌肉等软组织黏连,颏下、下颌下分别可见肿大淋巴结。在正常组织外将肿瘤完整摘除并同时行颏下、下颌下淋巴清扫术。结果病理(图2)检查,(左侧下颌骨)成软骨型骨肉瘤,颏下、下颌下淋巴结未见转移。(右下颌角区)慢性炎症。术后患者选择放疗治疗,随访1年未见复发与转移。

【讨论】
骨肉瘤是一种起源于骨间叶细胞的原发性恶性骨肿瘤,组织学类型可分为成骨细胞型、成软骨细胞型、成纤维细胞型、血管扩张型、骨旁型、骨膜型、小细胞型等。发病率低,恶性程度高。颌骨骨肉瘤少见,大部分发生于下颌骨,分化良好。Mardinger等报道颌骨骨肉瘤发病年龄在8~78岁之间,平均33岁;男性发病率略高于女性。发生于上颌骨者,女性居多;发生于下颌骨者,男性居多。大部分骨肉瘤的发病机制尚不明确,可能与基因突变有关,亦与放疗、Paget病、视网膜母细胞瘤、骨纤维异样增殖症等有关。生长发育似乎是长骨骨肉瘤的一个主要因素,却不是颌骨骨肉瘤的主要因素,因为颌骨骨肉瘤发病平均年龄约30~39岁,较长骨骨肉瘤平均晚10年。颌骨骨髓炎往往有牙痛史,急性期常伴有剧烈疼痛、高热等症状,慢性期疼痛缓解、体温可正常。而颌骨骨肉瘤常为无痛性肿胀,文献回顾显示,85%~95%的患者出现局部肿胀,45.8%~50%的患者出现疼痛。另外一些患者的主诉可能是感觉异常(21.2%),牙移位、松动、脱落,开口受限,鼻塞、鼻出血,眼球突出等。下颌骨骨肉瘤的X线呈现日光放射状表现(25%)。但对于一些早期骨肉瘤,往往很难出现这种表现,牙周膜间隙增宽被认为是骨肉瘤的一个早期影像学表现。Lindqvist等报道,X线片上下牙槽神经管及牙周间隙增宽及日光放射状表现是下颌骨骨肉瘤的特征性表现。骨髓炎亦可出现骨质吸收、增生以及牙周膜增宽现象,需与骨肉瘤相鉴别。CT和MRA在评价骨肉瘤的范围及与周围组织的关系方面具有重要价值。本病例CT显示,下颌骨左侧骨皮质粗糙,边缘密度不均匀,边界不清楚,表现成骨性改变;右侧下颌角区可见一阻生牙,周围骨质破坏,表现溶骨性改变,如图中箭头所指,可见骨皮质破坏(图1)。结合患者反复发作智牙冠周炎病史,考虑双侧同时分别为成骨性与溶骨性骨肉瘤的可能性极小,右侧骨髓炎的可能性大。病理检查结果(图2)也证明了术前的临床分析。另外,大部分骨肉瘤在影像学上仅表现为成骨性、溶骨性或混合性表现,无日光放射状等特征性表现,所以确诊仍需病理检查。组织学上,骨肉瘤由一些可以产生类骨质或不成熟骨质的梭形细胞组成。在下颌骨,约有一半以上来源于软骨分化。颌骨骨肉瘤在组织学上细胞分化往往较长骨者高,临床上有时很难辨别。因此,临床表现、影像学特点及组织学特性都是诊断颌骨骨肉瘤的重要依据。本病例为颌骨成软骨型骨肉瘤,与长骨成软骨型骨肉瘤不同的是,其预后较好,但是放疗后形成的颌骨骨肉瘤转移率较高,其预后有待于进一步研究。下颌骨骨肉瘤患者出现下唇麻木者较未出现者预后差。本病例无下唇麻木感,预测其预后较好。下颌骨骨肉瘤的治疗方式主要是切除下颌骨的根治性手术;如有淋巴结转移,还需行颈淋巴清扫术,术后行放疗、化疗可在一定程度上提高生存率。总之,其早期诊断和彻底手术是提高存活率的关键。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#下颌#
27
#骨髓炎#
39
#下颌骨#
38
学习
66
学习了受益匪浅
71