JAMA Oncol:怀孕会增加乳腺癌患者的死亡风险吗?
2017-03-18 peng wei 肿瘤资讯
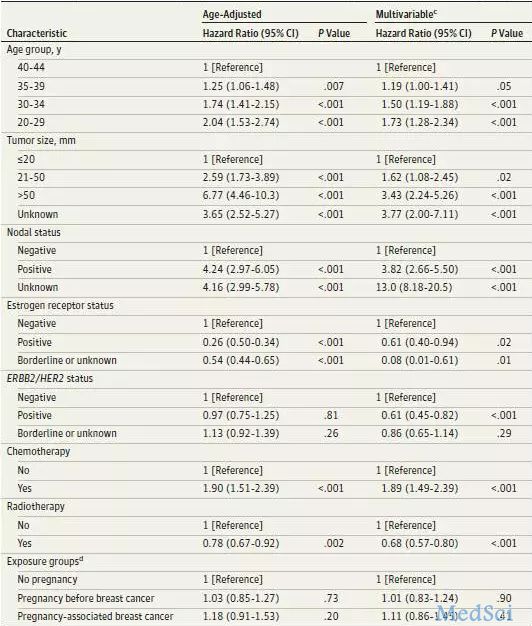
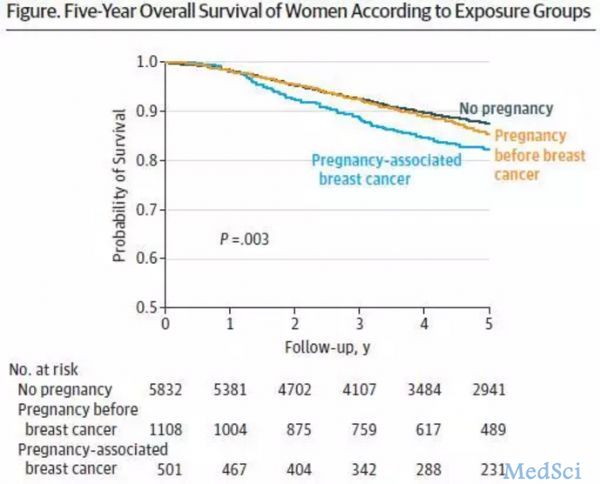
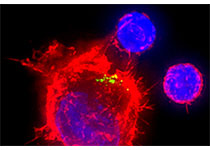
2016年美国约有247000名女性诊断为乳腺癌,其中包括26392名小于45岁的女性。近年来,首次分娩产妇年龄增长了5岁,超过35岁的产妇比例也增加。由于生育年龄的推迟,怀孕期间患乳腺癌的妇女(或接受治疗后计划怀孕的乳腺癌患者)比例增加。妊娠期(或分娩后1年)诊断为乳腺癌的患者均有一些临床病理特点,如肿瘤分级高,ER(雌激素受体),PR(孕激素受体)低表达。然而,怀孕是否会影响生存仍是一个争论的

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Oncol#
26
#死亡风险#
31
#乳腺癌患者#
31
这个研究方法值得学习
55
很好的学习资料,谢谢了。
56
学习了
53