European Radiology:克罗恩病中口服造影剂的类型和体积对MRE肠腔扩张程度的影响
2022-06-13 shaosai MedSci原创
肠道磁共振成像(MRE)无辐射,其依赖于良好的小肠扩张和多参数序列的结合以准确识别疾病和分型。
 众所周知,横断面成像对小肠克罗恩病(CD)的诊断和分期具有敏感性和特异性。肠道磁共振成像(MRE)无辐射,其依赖于良好的小肠扩张和多参数序列的结合以准确识别疾病和分型。诊断的准确性取决于管腔扩张的质量,不良的扩张影响诊断的准确性。肠道扩张程度受摄入的口服制剂的类型和数量的影响。
众所周知,横断面成像对小肠克罗恩病(CD)的诊断和分期具有敏感性和特异性。肠道磁共振成像(MRE)无辐射,其依赖于良好的小肠扩张和多参数序列的结合以准确识别疾病和分型。诊断的准确性取决于管腔扩张的质量,不良的扩张影响诊断的准确性。肠道扩张程度受摄入的口服制剂的类型和数量的影响。
虽然MRE通常耐受性良好,但与小肠超声(SBU)相比,其负担更重且会引起一定的不良症状,与口服制剂有关的胃肠道反映是MRE最不能被广泛接受的副作用之一,因此SBU通常被病人所青睐。
调查口服制剂的现有文献主要集中在单个中心的少数健康人身上[5, 10-15]。研究结果可能无法推广到接受MRE的(通常)有症状的病人。事实上,令人惊讶的是,很少有研究对患者的口服造影剂进行调查[16-17]。
近日,发表在European Radiology杂志的一项研究比较MRE和SBU对克罗恩病病变的范围和活动性的诊断准确性,为该类患者选择最佳的检查方法以及诊断结果准确性的保证提供了参考。
本研究是一项回顾性、观察性研究,研究对象是参加多中心、前瞻性试验的患者子集,评估了MRE对小肠克罗恩病的诊断准确性。来自105名患者(64名女性,平均年龄37岁)的整体和分段MRE小肠扩张程度,由两名经验丰富的观察者(68[65%]甘露醇和37[35%]PEG)打分,从0=差到4=优进行划分。此外,130名患者(77名女性,平均年龄34岁)完成了一份问卷对MRE后立即和2天的各种症状的耐受性进行评分(85[65%]接受甘露醇,45[35%]接受PEG)。使用比例检验法对不同药剂之间以及摄入≤1升甘露醇或>1升甘露醇的人之间的扩张程度进行比较。耐受性等级分为 "非常耐受"、"中等耐受 "和 "不耐受"。
甘露醇和PEG的每位患者的扩张程度相似("优秀 "或 "良好 "的比例分别为54%[37/68]和46%[17/37])。与PEG相比,甘露醇的空肠膨胀明显更好(40% [27/68] 对14% [5/37] 被评为优秀或良好)。摄入甘露醇的量没有明显差异。不同药物之间的症状耐受性相当,尽管在MRE之后,27%(12/45)摄入PEG的患者的饱胀感被评为 "非常耐受",而44%(37/84)摄入甘露醇,差异为17%(95% CI 0.6至34%)。
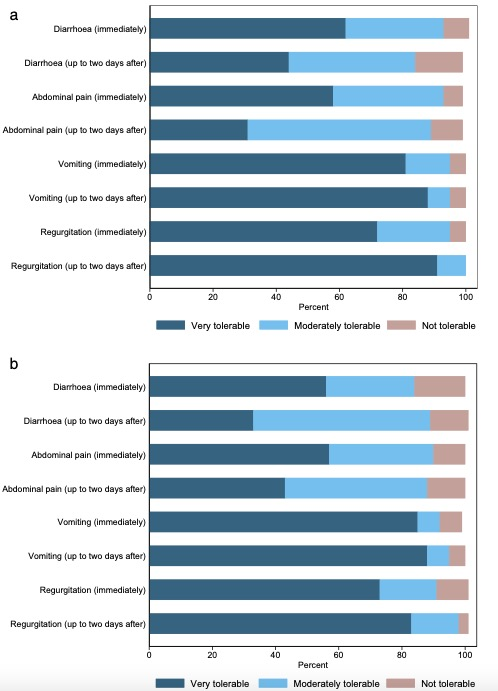
图 比较病人在MRE后立即及至2天内依赖(a)以甘露醇为基础和(b)以PEG为基础口服制剂的副作用症状
综上所述,甘露醇溶液和PEG可以达到适宜的扩张程度,且副作用的接受程度较高,但甘露醇的空肠扩张程度更显著。扩张程度不会因为摄入对比剂量超过1L而得到改善。
原文出处:
Gauraang Bhatnagar,Sue Mallett,Laura Quinn,et al.Influence of oral contrast type and volume on patient experience and quality of luminal distension at MR Enterography in Crohn's disease: an observational study of patients recruited to the METRIC trial.DOI:10.1007/s00330-022-08614-9
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#扩张#
34
#MRE#
48
#PE#
34
礼来
57
很不错
42
#造影#
44