Macromol Rapid Commun:同时具备抗菌成骨功能的复合微球可有效用于感染骨缺损的修复
2018-05-19 MedSci MedSci原创
骨缺损修复,尤其是感染方面,仍然是临床治疗中的一大挑战。为满足临床需要,同时具备抗菌活性和强大的骨生成效应的支架材料是骨组织工程中的一种有前景的方法。 在本研究中,研究人员制备了一种生物可吸收多孔结构微球体,由聚(I-丙交酯)和聚(乙二醇)嵌段组成的两亲嵌段共聚物制成。表面涂覆贻贝来源聚多巴胺后,通过依次生物矿化还原硝酸银和磷灰石,使微球载有纳米银。 将所制备的复合微球与大鼠骨间充质基
骨缺损修复,尤其是感染方面,仍然是临床治疗中的一大挑战。为满足临床需要,同时具备抗菌活性和强大的骨生成效应的支架材料是骨组织工程中的一种有前景的方法。
在本研究中,研究人员制备了一种生物可吸收多孔结构微球体,由聚(I-丙交酯)和聚(乙二醇)嵌段组成的两亲嵌段共聚物制成。表面涂覆贻贝来源聚多巴胺后,通过依次生物矿化还原硝酸银和磷灰石,使微球载有纳米银。
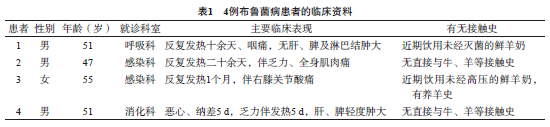
将所制备的复合微球与大鼠骨间充质基质细胞和金黄色葡萄球菌的体外共培养来系统地评估复合微球的细胞毒性和抗菌活性。最后将复合微球体填充到大鼠感染的颅骨缺陷模型中进行体内评估。
综上所述,改研究结果表明,多功能微球可在促进骨再生的同时具备抗感染的能力。
原始出处:
Wei P1, Yuan Z, et al., Bioresorbable Microspheres with Surface-Loaded Nanosilver and Apatite as Dual-Functional Injectable Cell Carriers for Bone Regeneration. Macromol Rapid Commun. 2018 May 11:e1800062. doi: 10.1002/marc.201800062.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#COMMUN#
20
#MAC#
23
#CRO#
18
#抗菌#
24
#成骨#
30
#ACR#
21
#骨缺损#
22