N Engl J Med:度鲁特韦(Dolutegravir)作为儿童HIV-1感染的一线或二线治疗优于标准治疗
2022-01-01 MedSci原创 MedSci原创
在世界范围内,估计有180万15岁以下的儿童和青少年感染人类免疫缺陷病毒(HIV)。人类免疫缺陷病毒1型(HIV-1)感染儿童有效抗逆转录病毒治疗(ART)的选择有限,结局始终较差。度鲁特韦是一种第二
在世界范围内,估计有180万15岁以下的儿童和青少年感染人类免疫缺陷病毒(HIV)。人类免疫缺陷病毒1型(HIV-1)感染儿童有效抗逆转录病毒治疗(ART)的选择有限,结局始终较差。度鲁特韦是一种第二代HIV整合酶链转移抑制剂(INSTI),已在涉及成人的试验中显示有效,并正在国家治疗项目中迅速推出。
实验方法:
我们进行了一项开放性、随机、非劣效性试验,在开始一线或二线ART的儿童和青少年中比较了基于HIV整合酶抑制剂度鲁特韦的三药ART与标准治疗(非度鲁特韦ART)。主要终点是96周时病毒学或临床治疗失败的受试者比例,通过Kaplan–Meier方法估计。同时评估安全性。
实验结果:
从2016年9月至2018年6月,共有707名体重至少14 kg的儿童和青少年被随机分配接受基于Dolutegravir的ART(350名参与者)或标准治疗(357名)。中位年龄为12.2岁(范围:2.9-18.0),中位体重为30.7 kg(范围:14.0-85.0),49%的受试者为女孩。
根据设计,311例受试者(44%)开始一线ART(标准治疗组92%的受试者接受基于依法韦仑的ART),396例(56%)开始二线ART(标准治疗组98%的受试者接受基于增强蛋白酶抑制剂的ART)。中位随访时间为142周。
到96周时,Dolutegravir组47例受试者和标准治疗组75例受试者治疗失败(估计概率,0.14 vs. 0.22;差异,-0.08;95%置信区间,-0.14至-0.03;P = 0.004)。一线和二线治疗的治疗效果相似(异质性P = 0.16)。(见图1和表2)
Dolutegravir组和标准治疗组分别共有35例和40例受试者发生至少1起严重不良事件(P = 0.53),分别有73例和86例受试者发生至少1起≥3级不良事件(P = 0.24)。Dolutegravir组和标准治疗组分别有5例和17例受试者发生至少1例ART修饰不良事件(P = 0.01)。(见表4)
在接受一线治疗的受试者(ODYSSEY A队列)中,Dolutegravir组在治疗失败后均未发生重大耐药突变(根据国际AIDS协会的定义)。在标准治疗组的29例参与者中,截至第96周病毒学治疗失败,且治疗后失败耐药性检测可用于该药物类别,18例参与者(62%)有NRTI相关突变,27例(93%)有NNRTI相关突变,没有蛋白酶抑制剂相关突变;大多数突变是新的。(见表3)
图1:在48、96和144周时病毒学或临床治疗失败的参与者比例的差异
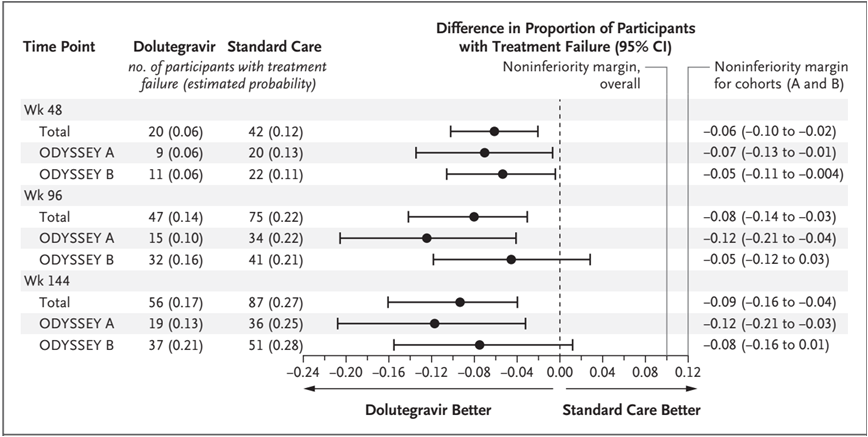
表2:以Dolutegravir为基础的ART与标准治疗疗效终点比较
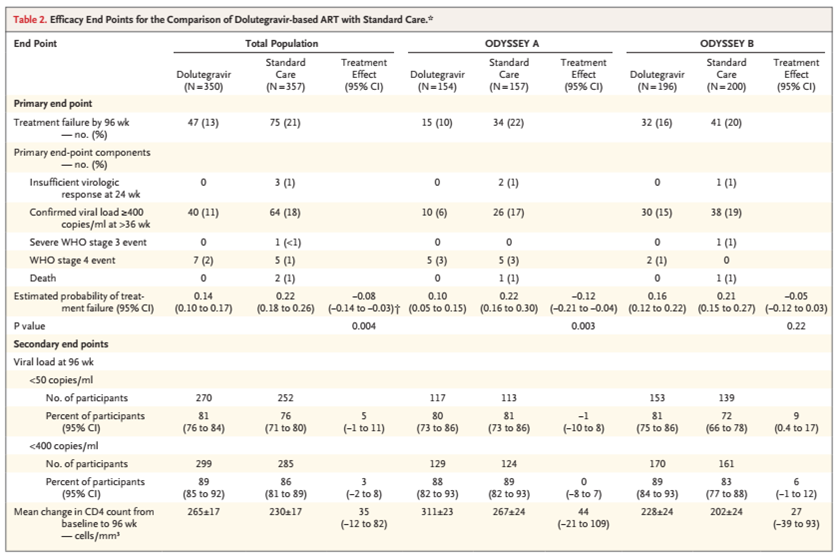
表3:基于Dolutegravir的ART和标准治疗的基因型耐药性比较

表4:基于Dolutegravir的ART与标准治疗的安全性终点比较

结论:
在这项涉及开始一线或二线治疗的HIV-1感染儿童和青少年的试验中,基于Dolutegravir的ART优于标准治疗。
原文链接:https://pubmed.ncbi.nlm.nih.gov/34965338/
Dolutegravir as First- or Second-Line Treatment for HIV-1 Infection in Children
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#标准治疗#
44
#度鲁特韦#
37
#Dolutegravir#
42
#Engl#
64
#Eng#
55
#二线治疗#
49
#Med#
37