JAMA:红细胞输注或可增加PCI术后心脏不良事件风险
2014-03-04 坞霜降 dxy
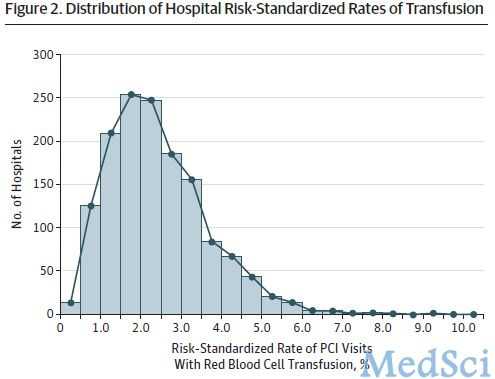
有研究指出在急性冠脉综合征患者中,红细胞输注使用情况存在一定的差异。同时,在冠心病治疗中,红细胞输注方案本身就备受争议。目前没有确凿的证据阐述该方案的治疗作用,另一方面,也没有相关数据可以证明该方案的不良作用。【原文下载】而事实上,尽管对于红细胞输注尚存争议,临床医生在经皮冠状动脉介入治疗(PCI)中还是会对部分患者进行红细胞输注。但是,我们必须面对的事实是:我们并没有完全掌握这种治疗方式的利弊与
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#PCI术#
30
#不良事件风险#
29
#红细胞输注#
41
#心脏不良事件#
42
#红细胞#
45
#PCI术后#
30