Front Oncol:围手术期化疗与胃肝样腺癌(HAS)患者预后的关系
2022-02-04 yd2015 MedSci原创
研究表明,基于铂和氟尿嘧啶的NAC可能不能改善局部晚期HAS患者的总生存期(OS)和无病生存期(DFS)。接受≧6个周期辅助化疗的患者生存率较高。
胃肝样腺癌(HAS)是胃癌的一种少见亚型,围手术期化疗对HAS的作用仍知之甚少。因此,北京大学肿瘤医院团队开展了回顾性研究,目的是探讨围手术期化疗与HAS患者预后的关系。相关结果发表在Frontiers in Oncology杂志上。
我们回顾性分析了2009年11月至2020年10月在北京大学肿瘤医院接受根治性手术的局部进展期HAS患者。将患者分为新辅助化疗优先组(NAC-first)和手术优先组。采用单因素、多因素生存分析和倾向评分匹配分析(PSM)分析围手术期化疗与HAS预后的关系。
共纳入100例患者进行分析,其中NAC组29例,手术组71例。PSM(1:1)后共纳入56例患者。HAS患者中Her-2阳性表达率(免疫组化3+染色或荧光原位杂交阳性)为22.89%(19/83)。在手术组中,23%(14/61)的患者Her-2阳性,NAC组为22.7%(5/22)。 NAC组的III/ IVa期患者比例明显高于手术优先组(100% vs 78.9%, P=0.01)。然而,手术优先组的淋巴血管侵犯比NAC优先组更为普遍(67.6% vs 44.8%, P=0.03)。神经侵犯水平相似(63.4% vs 41.4%,P=0.04)。
29例患者行NAC。其中,S-1+奥沙利铂(SOX) 19例,奥沙利铂+卡培他滨(XELOX) 6例,SOX+紫杉醇+曲妥珠单抗1例,XELOX+曲妥珠单抗1例,多西他赛+顺铂+氟尿嘧啶(DCF) 1例,奥沙利铂+亚叶酸钙+氟尿嘧啶(mFOLFOX) 1例。中位周期数为3个周期(1 ~ 5个周期)。NAC组治疗部分缓解(PR) 6例,病情稳定(SD) 20例,病情进展(PD) 1例,完全缓解(CR) 1例。NAC组治疗后4例为肿瘤衰退1级(TRG1), 4例诊断为TRG2, 19例诊断为TRG3。
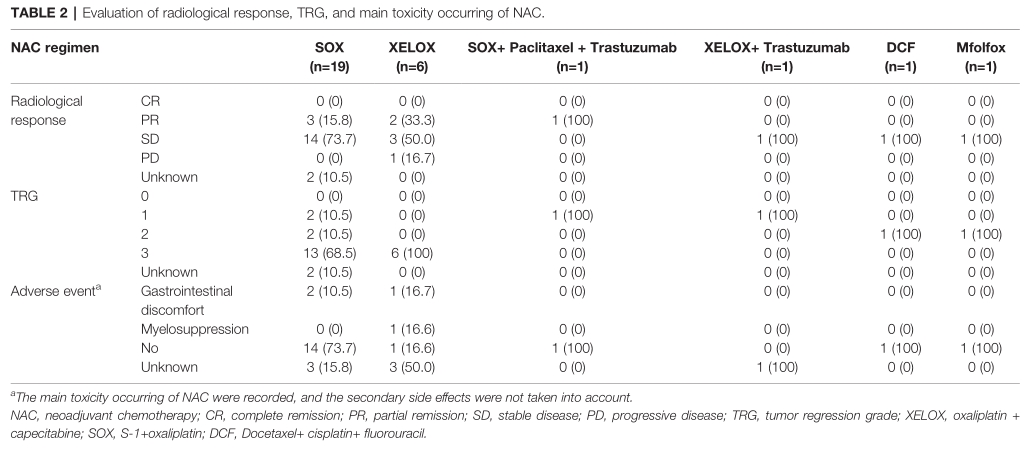
疗效评估
PSM前,手术优先组的OS优于NAC优先组( P=0.02)。 NAC组1,3年OS率分别为92.7% 和68.2%,手术组分别为 97% 和83.4%。PSM后,两组的OS没有显著统计学差异( P=0.105)。同样,PSM前手术优先组的DFS时间明显长于NAC优先组(P=0.022)。NAC组1年和3年DFS率分别为80.4%和71.5%;手术组1年和3年DFS率分别为97%和83.8%。PSM后,两组的DFS没有显著统计学差异(P=0.108)。
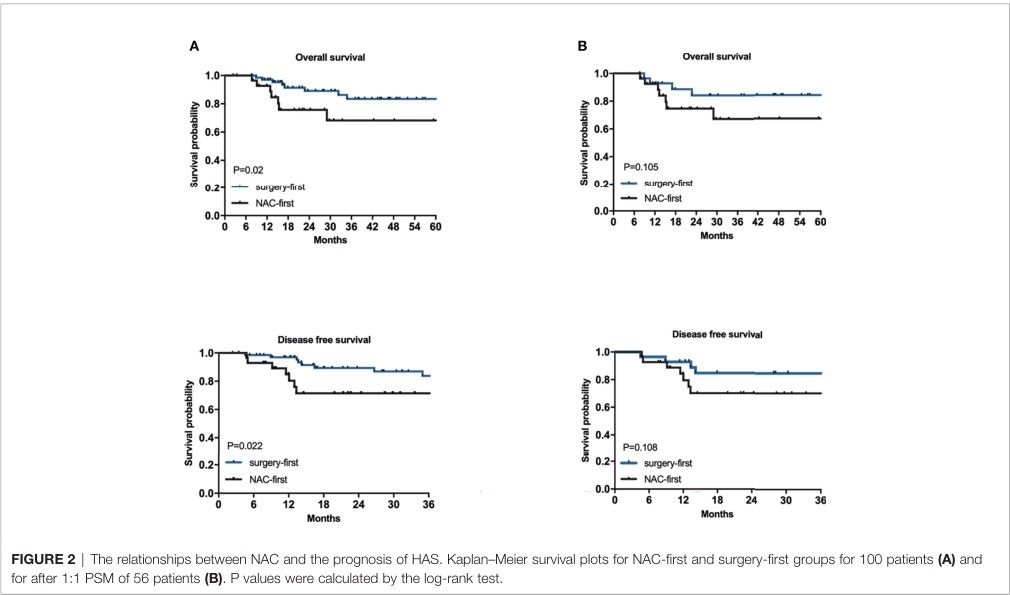
PSM前后OS和DFS
我们还分析了辅助化疗周期数与HAS患者预后的关系。在61例先行手术的患者中,我们发现≧6个周期组的OS(P=0.023)和DFS(P=0.013)均优于<6个周期组。
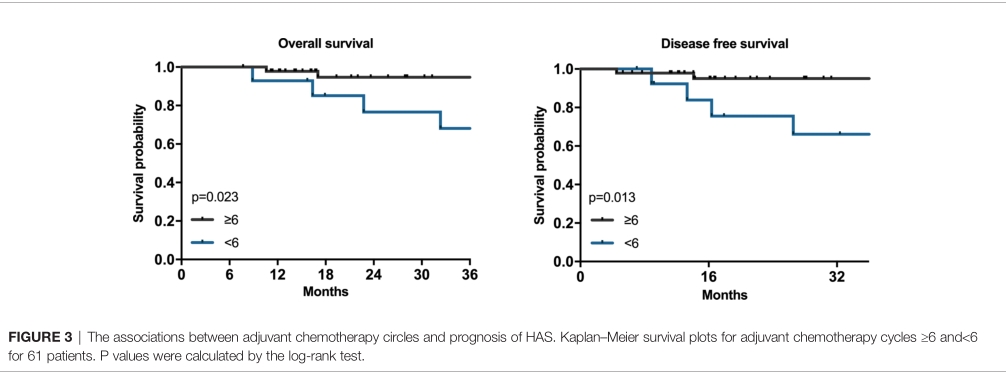
辅助化疗周期数和OS、DFS关系
综上,研究表明,基于铂和氟尿嘧啶的NAC可能不能改善局部晚期HAS患者的总生存期(OS)和无病生存期(DFS)。接受≧6个周期辅助化疗的患者生存率较高。因此,对于局部进展期的HAS,建议采用根治性胃切除术联合充分的辅助化疗治疗。
原始出处:
Zhou K, Wang A, Wei J, Ji K, Li Z, Ji X, Fu T, Jia Z, Wu X, Zhang J and Bu Z (2022) The Value of Perioperative Chemotherapy for Patients With Hepatoid Adenocarcinoma of the Stomach Undergoing Radical Gastrectomy. Front. Oncol. 11:789104.doi: 10.3389/fonc.2021.789104
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#患者预后#
47
#手术期#
45
#Oncol#
30
学术经验
56