再生医学是一个快速发展的领域,有可能为难以治疗的疾病提供创新疗法。许多治疗依赖于使用干细胞或细胞疗法,但这些手段在技术上都具有挑战性并且生产成本很高。为了解决这个问题,许多生物技术公司正在寻找替代方法来提高再生医学治疗的功效,同时降低成本,并提高可及性。
使用多肽等新疗法提供了一种不同的方法,这些多肽可以刺激身体自身的细胞在损伤部位进行修复和再生,同时避免体外细胞培养所涉及的不确定性。开发再生肽提供了一个令人兴奋的机会,可以以负担得起的、可获得的和可预测的方式帮助患者。
干细胞治疗面临挑战:
干细胞疗法已用于广泛的生物医学应用,从用皮肤移植治疗烧伤患者,到通过将间充质干细胞注射到受影响的关节中来改善骨关节炎症状。然而,迄今为止,成功的案例并不多见。治疗结果通常不一致,患者之间的差异很大,部分原因是干细胞的脆弱性。尽管随着时间的推移,对它们的特性和培养条件的了解有所改善,但干细胞仍可能会改变其表面标志物,并在细胞生长和分裂过程中失去自我更新和分化的能力,从而降低治疗效果。
干细胞的来源也面临伦理争议。如今,最常见的是诱导多能干细胞或造血干细胞(从脐带血中提取和衍生的干细胞),但这些细胞很难生产。此外,只有专业的医疗中心或设施才能满足细胞生长所需的高度特殊的条件。这意味着为一个疗程产生和维持足够的干细胞的成本往往很高,从而降低了患者的可及性。
为了应对干细胞研究所面临的挑战,许多生物技术公司正在研究可以诱导组织再生以修复损伤和恢复身体功能的其他药物或治疗方法。
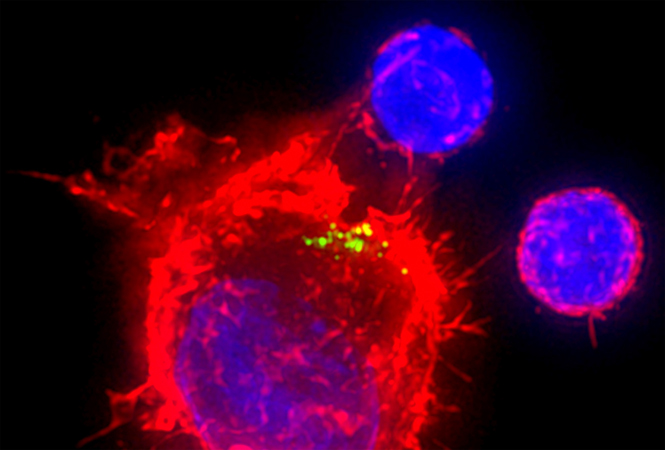
再生医学的另一种方法是使用新型肽来刺激和再生患者自身的干细胞,以加速愈合过程并修复受损组织。例如,色素上皮衍生因子 (PEDF) 是一种多功能蛋白质,已知具有抗炎和抗血管生成功能,这意味着它可以抑制新血管的生长。此外,PEDF具有支持神经元生长、存活的能力。许多研究表明,一种称为 PEDF 衍生的短肽 (PDSP),可以促进角膜缘上皮干细胞以及睑板腺干细胞的生长和扩增。因此,它可以通过刺激角膜干细胞增殖和分化、抗炎和睑板腺恢复来加速角膜修复过程,从而用于治疗干眼症。
PDSP 还被证明可以促进间充质干细胞的生长,这些干细胞可以分化成多种组织类型,包括骨骼、软骨、肌肉和脂肪细胞以及结缔组织。因此,它有可能通过促进软骨再生、修复损伤和缓解关节疼痛来治疗其他疾病,例如骨关节炎。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















学习
61
#多肽#
56
学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习
69
Zbc
55
丿寸⺌出学
62
点击[http://img01.sogoucdn.com/app/a/200678/1fc21ebc11704cf8593e69ffdd7bc081.gif]查看表情
52