Cancer Cell:内皮细胞Notch 1活性促进肿瘤转移
2017-06-14 海北 MedSci原创
肿瘤转移一直是癌症治疗中最令人头疼的事儿之一。对其机制的研究也是层出不穷。6月13日,德国科学家Andreas Fischer在肿瘤细胞(Caner Cell)上发文阐释内皮细胞和肿瘤转移之间的关系。
肿瘤转移一直是癌症治疗中最令人头疼的事儿之一。对其机制的研究也是层出不穷。6月13日,德国科学家Andreas Fischer在肿瘤细胞(Caner Cell)上发文阐释内皮细胞和肿瘤转移之间的关系。
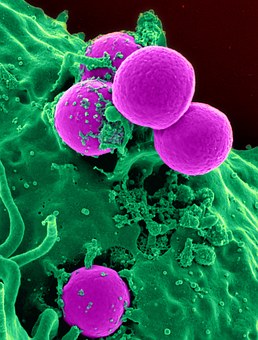
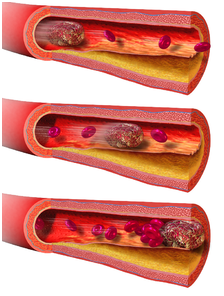
内皮细胞能够产生血管分泌因子,协调肿瘤进展。Andreas Fischer课题组发现,在人类癌症和黑色素瘤的内皮细胞中,以及小鼠转移前肿瘤微环境中的内皮细胞上,经常能观察到活化的Notch 1受体。在黑色素瘤中,内皮细胞Notch 1受体的表达和较短的无进展生存期相关。此外,持续的Notch 1活化能够诱导内皮细胞的衰老,促使其表达趋化因子以及粘附因子VCAM 1。这会进一步促进嗜中性粒细胞的浸润,肿瘤细胞在内皮上的粘附、渗透、在肺部的聚集,以及术后转移。因此,种种迹象表明,持续的血管Notch信号激活通过产生一个衰老的促炎性内皮来促进肿瘤转移。
进而,利用Notch 1或是VCAM 1的阻断抗体治疗可以预防Notch诱导的肿瘤转移。在卵巢癌的小鼠模型中,利用基因手段破坏内皮细胞的Notch信号通路也可以抑制腹膜中性粒细胞的浸润。
原始出处:
Elfriede Wieland et al. Endothelial Notch1 Activity Facilitates Metastasis. 2017, Cancer Cell 31, 355–367. DOI: http://dx.doi.org/10.1016/j.ccell.2017.01.007
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CEL#
22
#cancer cell#
31
#Cell#
29
#肿瘤转移#
31
#Notch#
23
#OTC#
28