Nat Commun:食管鳞状细胞癌中诱导化疗结合根治性放化疗与单独放化疗的疗效比较
2021-07-01 xiaozeng MedSci原创
食管癌(EC)作为全球癌症相关死亡的第六大原因,是一种预后不佳的致命性疾病。
食管癌(EC)作为全球癌症相关死亡的第六大原因,是一种预后不佳的致命性疾病。既往研究显示,同步放化疗(CRT)是不适合手术的EC患者的一种标准护理策略。
尽管近年来的放疗和化疗方案已取得了一定的进展,但接受CRT治疗的患者的预后仍不乐观,患者的3年总生存率(OS)仅为26.9–55.4%。更重要的是,超过50%的患者在针对性CRT后发生了疾病的局部或远端复发。因此,急需更有效的治疗方案。
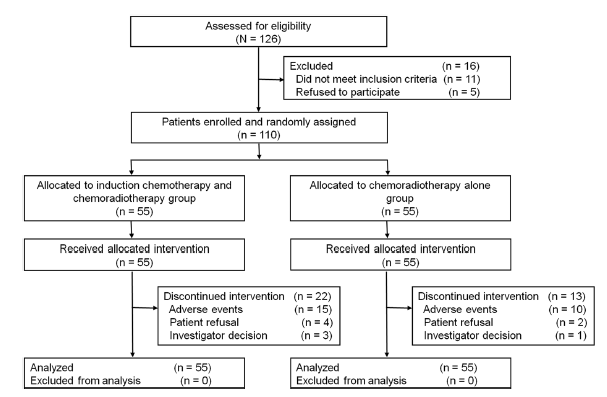
该项随机性II期临床试验旨在比较诱导化疗继以根治性放化疗(CRT)与单独的CRT治疗在不适合手术的ESCC(食管鳞状细胞癌)患者中的疗效和安全性(患者数量N=110)。该试验的主要结局为总体反应率(ORR),次要结局是总生存期。
相关研究示意图
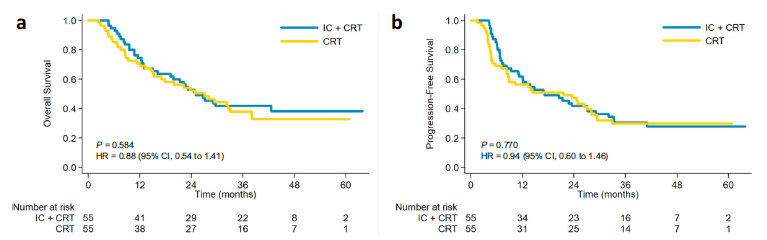
结果显示,该试验并未达到预先指定的终点。诱导化疗组的ORR为74.5%,而单独CRT治疗组的ORR为61.8%(P值为0.152)。诱导化疗组患者的3年总生存率为41.8%,而单独CRT组为38.1%(P值为0.584,风险比为0.88)。两组患者的3-5级不良事件相似。事后分析显示,对诱导化疗有反应的患者的生存率有所提高。
两个治疗组的Kaplan-Meier生存曲线
总而言之,该研究结果揭示,对于ESCC患者,在CRT治疗的基础上加入诱导化疗并不能改善患者的药物反应率或生存率。
原始出处:
Liu, S., Luo, L., Zhao, L. et al. Induction chemotherapy followed by definitive chemoradiotherapy versus chemoradiotherapy alone in esophageal squamous cell carcinoma: a randomized phase II trial. Nat Commun 12, 4014 (29 June 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Nat#
35
#细胞癌#
37
#COMMUN#
44
#放化疗#
33
#食管鳞状细胞癌#
66
#食管#
36
#诱导化疗#
0
#根治#
32
好好学习天天向上
62
谢谢梅斯提供这么好的信息,学到很多
51