JAMA:直肠癌患者:腹腔镜手术vs开腹手术
2015-10-09 Mechront 译 MedSci原创
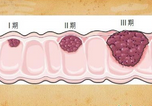
目前对经腹腔镜行直肠癌切除术的有效性评价不一,尤其是晚期直肠癌。研究者进行了一项多中心双盲的随机对照试验,欲探究对于直肠癌患者行切除术,究竟是选择腹腔镜好,还是开腹手术更优,以大体标本和切除后组织结果作为评判。该研究于2008.10-2013.09在美国和加拿大的35个中心进行,共纳入486名临床分期为II、III期、距离肛门外源12cm以内的直肠癌患者,完成新辅助化疗后,随机分为腹腔镜组(n=2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













好,谢谢
171
Ok
105
感谢作者分享
113
#腹腔镜#
32
#腹腔镜手术#
43
比较下来是没有明显差异的意思么
129