JAMA子刊:别小瞧贫血,或可导致听力损失!
2017-01-09 生物探索 生物探索
导读:听力损伤或许是由缺铁性贫血所导致,来自宾夕法尼亚州立大学医学院的Kathleen M. Schieffer领导的研究团队详细地探究了缺铁性贫血与听力损失的关系。该研究发表于JAMA Otolaryngology - Head & Neck Surgery杂志上。在美国,约有15%的成年人都受到一定程度的听力损失的影响。其中,三分之二以上的成年人超过65岁,80%的成年人超过85岁。听
导读:听力损伤或许是由缺铁性贫血所导致,来自宾夕法尼亚州立大学医学院的Kathleen M. Schieffer领导的研究团队详细地探究了缺铁性贫血与听力损失的关系。该研究发表于JAMA Otolaryngology - Head & Neck Surgery杂志上。
在美国,约有15%的成年人都受到一定程度的听力损失的影响。其中,三分之二以上的成年人超过65岁,80%的成年人超过85岁。听力损失与健康状况不佳,高血压,吸烟,糖尿病和住院密切相关。
由于听力损失可能对个人健康产生重大影响,并且病因尚不明确,因此科学家们正在探索新的风险因素。比如,在突发性感音神经性听力损失(SNHL)中,患者听力在72小时内严重减少,最近研究表明该病与缺铁性贫血(IDA)相关。来自宾夕法尼亚州立大学医学院的Kathleen M. Schieffer领导的研究团队详细地探究了IDA与听力损失的关系。该研究发表于JAMA Otolaryngology - Head & Neck Surgery杂志上。
缺铁性贫血和听力损失
IDA是由身体缺铁引起的常见病症,其导致红细胞数目减少。由于红细胞负责在机体中运送氧气,因此IDA减少了可被组织利用的氧气含量。在全世界范围内,IDA影响着数亿人,其中美国的IDA患者估计有500万人。
研究团队使用来自Hershey医疗中心的电子医疗记录的数据。总共调查了来自305,339名21-90岁的成年人的数据,其中43%是男性,平均年龄为50岁。通过观察铁蛋白和血红蛋白水平,回顾性诊断IDA。
贫血如何影响听力?
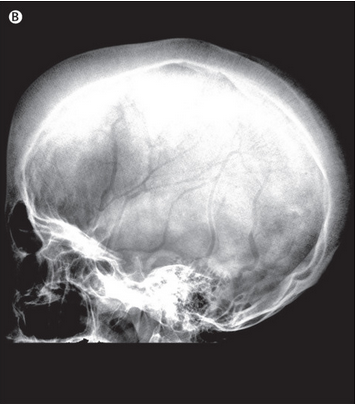
为何IDA与听力损失相关?这其中的具体机制科学家尚未完全了解,但是存在一些可能的途径。比如,血液经由迷路动脉供应到内耳,这一过程对缺血性损伤(由血流量减少引起的损伤)高度敏感。因此可能成为贫血影响听力的原因之一。此外,具有血管疾病的人群更容易受患突发性SNHL。因此,血液供应显然是听力损失的一个重要因素。
另一种可能的机制涉及到髓磷脂,髓磷脂时一种附着在神经上的蜡质物质,它对于神经纤维的信号传导效率至关重要。体内缺铁引起脂质饱和酶及去饱和酶的降解,这两者在能量生产及髓磷脂的合成过程中十分重要。如果髓鞘包裹听神经的过程受损,听力可能降低。
研究小组的下一步计划将是观察铁补充是否可能积极干预听力损失。如果它确实可以改善受损的听力或减少听力损失,那么,这将可能成为一种既划算又有效的治疗方式。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












保护好自己的听力很重要
48
收藏了,谢谢分享
51
受益匪浅
53
继续学习中
60
#听力#
24
收藏
42