Nat Commun:日研究找到易被特定癌细胞吸收的肽
2012-07-23 新华网 新华网
新一期英国在线科学期刊《自然—通讯》(Nature Communications)发表了日本的一个研究小组的研究报告,他们发现了大肠癌、乳腺癌、白血病(俗称“血癌”)等10种癌细胞容易吸收的肽,这将有助于这些癌症的早期发现与治疗。 综合日本媒体报道,日本爱知县癌症中心研究所、琉球大学等机构的研究人员以溶液中氨基酸排列方式不同的1万亿种肽为对象,研究各种癌细胞对它们吸收的难易程度,结果发现白血病细

新一期英国在线科学期刊《自然—通讯》(Nature Communications)发表了日本的一个研究小组的研究报告,他们发现了大肠癌、乳腺癌、白血病(俗称“血癌”)等10种癌细胞容易吸收的肽,这将有助于这些癌症的早期发现与治疗。
综合日本媒体报道,日本爱知县癌症中心研究所、琉球大学等机构的研究人员以溶液中氨基酸排列方式不同的1万亿种肽为对象,研究各种癌细胞对它们吸收的难易程度,结果发现白血病细胞容易吸收肽CPP44。
研究人员让能够抑制癌细胞增殖的抗癌物质与CPP44结合,以治疗患白血病的实验鼠。结果,实验鼠体内的癌细胞得以更充分地吸收抗癌物质,癌组织缩小到原先的50%至30%,实验鼠生存时间有所延长。同时,这种治疗未引发明显的副作用。
通过这项研究,科研人员找到了大肠癌、乳腺癌、肺癌等10种癌细胞容易吸收的特定种类的肽。参与研究的肿瘤病理学专家近藤英作介绍说,此前研究者发现易被癌细胞吸收的肽同时也易被正常细胞吸收,找到只容易被癌细胞吸收的肽十分不易。
研究人员指出,利用这些肽承担抗癌药物“搬运工”,能使药物被集中送达癌细胞,有助于抑制副作用。另外,即使肿瘤体积还很小,如果让这些肽与色素相结合并注入肌体,就能使肿瘤组织变色且便于观察,从而帮助尽早发现癌症。

doi:10.1038/ncomms1952
PMC:
PMID:
Tumour lineage-homing cell-penetrating peptides as anticancer molecular delivery systems
Eisaku Kondo,1, 2 Ken Saito,1 Yuichi Tashiro,3 Kaeko Kamide,4 Shusei Uno,4 Tomoko Furuya,5 Masao Mashita,6 Kiichiro Nakajima,7 Tomoyuki Tsumuraya,8 Naoya Kobayashi,9 Masahiro Nishibori,10 Mitsune Tanimoto11 & Masayuki Matsushita8
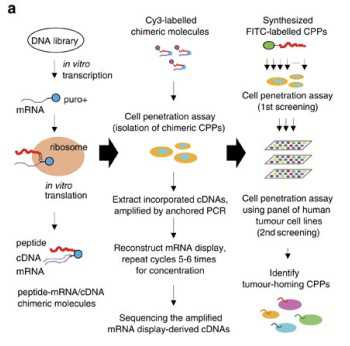
Cell-penetrating peptides have gained attention owing to their promise in noninvasive delivery systems. Among the identified cell-penetrating peptides, the TAT peptide has been preferentially used for transduction into cells of diverse origins. However, this activity is nonselective between neoplastic and non-neoplastic cells. Here we describe artificial cell-penetrating peptides that are selectively and efficiently incorporated into human tumour cells, according to their lineage. Ten representative tumour lineage-homing cell-penetrating peptides were obtained by screening of a random peptide library constructed using messenger RNA display technology, and some of the isolates were further modified by amino-acid substitution. Their advantageous tumour cell-targeting ability is corroborated in an in vivo mouse model for imaging and growth suppression of metastatic xenoplant tumours. These cell-penetrating peptides are potentially useful for the efficient targeting of human neoplasms in a tumour origin-dependent manner, and provide a framework for the development of peptide-based anti-tumour technologies.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#COMMUN#
47
#Nat#
43
#细胞吸收#
30
#癌细胞#
34